1. Aiken C, “A Potentially Lethal Side Effect You’ve Probably Never Heard Of.” The Carlat Psychiatry Report [Internet] 2020 May [cited 2020 Sep 3] [cited 2022 June 24]
2. Spielmans G, “Olanzapine No Better than Placebo for Borderline Personality Disorder.” The Carlat Psychiatry Report [Internet] 2009 Feb [cited 2020 Sep 3] [cited 2022 June 24]
3. Cadario B. Olanzapine (Zyprexa): suspected serious reactions. CMAJ. 2000 Jul 11;163(1):85-6, 89-90. English, French. PMID: 10920744. [cited 2022 June 24]
4. “Summary Safety Review – Atypical antipsychotics – Assessing the potential risk of Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)” published by Health Canada [Internet] 2018 Apr 10 [cited 2020 Sep 3] [cited 2022 June 24]
5. Zyprexa (olanzapine) label FDA [approval 1996] [cited 2022 June 24]
6. Hempel S, Taylor SL, Solloway MR, et al. Evidence Map of Acupuncture [Internet]. Washington (DC): Department of Veterans Affairs (US); 2014 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK185076/ [cited 2022 June 24]
7. Andres K, Bellwald L, Brenner HD. Empirische Untersuchung einer leiborientierten Therapie mit schizophrenen Patienten [Empirical study of a physically oriented therapy with schizophrenic patients]. Z Klin Psychol Psychopathol Psychother. 1993;41(2):159-69. German. PMID: 8511959. [cited 2022 June 24]
8. Corring D, Lundberg E, Rudnick A. Therapeutic horseback riding for ACT patients with schizophrenia. Community Ment Health J. 2013 Feb;49(1):121-6. doi: 10.1007/s10597-011-9457-y. Epub 2011 Oct 21. PMID: 22015959. [cited 2022 June 24]
9. Girdler SJ, Confino JE, Woesner ME. Exercise as a Treatment for Schizophrenia: A Review. Psychopharmacol Bull. 2019 Feb 15;49(1):56-69. PMID: 30858639; PMCID: PMC6386427. [cited 2022 June 24]
10. Health Quality Ontario. Cognitive Behavioural Therapy for Psychosis: A Health Technology Assessment. Ont Health Technol Assess Ser. 2018 Oct 24;18(5):1-141. PMID: 30443277; PMCID: PMC6235075. [cited 2022 June 24]
11. Aucoin M, LaChance L, Clouthier SN, Cooley K. Dietary modification in the treatment of schizophrenia spectrum disorders: A systematic review. World J Psychiatry. 2020 Aug 19;10(8):187-201. doi: 10.5498/wjp.v10.i8.187. PMID: 32874956; PMCID: PMC7439299. [cited 2022 June 24]
12. Aucoin M, LaChance L, Cooley K, Kidd S. Diet and Psychosis: A Scoping Review. Neuropsychobiology. 2020;79(1):20-42. doi: 10.1159/000493399. Epub 2018 Oct 25. PMID: 30359969. [cited 2022 June 24]
13. Adan RAH, van der Beek EM, Buitelaar JK, Cryan JF, Hebebrand J, Higgs S, Schellekens H, Dickson SL. Nutritional psychiatry: Towards improving mental health by what you eat. Eur Neuropsychopharmacol. 2019 Dec;29(12):1321-1332. doi: 10.1016/j.euroneuro.2019.10.011. Epub 2019 Nov 14. PMID: 31735529. [cited 2022 June 24]
14. Cabral P, Meyer HB, Ames D. Effectiveness of yoga therapy as a complementary treatment for major psychiatric disorders: a meta-analysis. Prim Care Companion CNS Disord. 2011;13(4):PCC.10r01068. doi: 10.4088/PCC.10r01068. PMID: 22132353; PMCID: PMC3219516. [cited 2022 June 24]
15. Cavaleri F. Review of Amyotrophic Lateral Sclerosis, Parkinson’s and Alzheimer’s diseases helps further define pathology of the novel paradigm for Alzheimer’s with heavy metals as primary disease cause. Med Hypotheses. 2015 Dec;85(6):779-90. doi: 10.1016/j.mehy.2015.10.009. Epub 2015 Oct 19. Erratum in: Med Hypotheses. 2017 Jan;98:5. PMID: 26604027. [cited 2022 June 24]
16. Ayuso-Álvarez A, Simón L, Nuñez O, Rodríguez-Blázquez C, Martín-Méndez I, Bel-Lán A, López-Abente G, Merlo J, Fernandez-Navarro P, Galán I. Association between heavy metals and metalloids in topsoil and mental health in the adult population of Spain. Environ Res. 2019 Dec;179(Pt A):108784. doi: 10.1016/j.envres.2019.108784. Epub 2019 Sep 28. PMID: 31606614. [cited 2022 June 24]
17. Ma J, Yan L, Guo T, Yang S, Guo C, Liu Y, Xie Q, Wang J. Association of Typical Toxic Heavy Metals with Schizophrenia. Int J Environ Res Public Health. 2019 Oct 30;16(21):4200. doi: 10.3390/ijerph16214200. PMID: 31671526; PMCID: PMC6862006. [cited 2022 June 24]
18. Flanagan MF. The Role of the Craniocervical Junction in Craniospinal Hydrodynamics and Neurodegenerative Conditions. Neurol Res Int. 2015;2015:794829. doi: 10.1155/2015/794829. Epub 2015 Nov 30. PMID: 26770824; PMCID: PMC4681798. [cited 2022 June 24]
19. Nurenberg JR, Schleifer SJ, Shaffer TM, Yellin M, Desai PJ, Amin R, Bouchard A, Montalvo C. Animal-assisted therapy with chronic psychiatric inpatients: equine-assisted psychotherapy and aggressive behavior. Psychiatr Serv. 2015 Jan 1;66(1):80-6. doi: 10.1176/appi.ps.201300524. Epub 2014 Oct 31. PMID: 25269512. [cited 2022 June 24]
20. Chu CI, Liu CY, Sun CT, Lin J. The effect of animal-assisted activity on inpatients with schizophrenia. J Psychosoc Nurs Ment Health Serv. 2009 Dec;47(12):42-8. doi: 10.3928/02793695-20091103-96. PMID: 20000282. [cited 2022 June 24]
21. Dayabandara M, Hanwella R, Ratnatunga S, Seneviratne S, Suraweera C, de Silva VA. Antipsychotic-associated weight gain: management strategies and impact on treatment adherence. Neuropsychiatr Dis Treat. 2017;13:2231-2241. Published 2017 Aug 22. doi:10.2147/NDT.S113099 [cited 2022 June 24]
22. Rada P, Avena NM, Hoebel BG. Daily bingeing on sugar repeatedly releases dopamine in the accumbens shell. Neuroscience. 2005;134(3):737-44. doi: 10.1016/j.neuroscience.2005.04.043. PMID: 15987666. [cited 2022 June 24]
23. Brown HE, Roffman JL. Vitamin supplementation in the treatment of schizophrenia. CNS Drugs. 2014;28(7):611-622. doi:10.1007/s40263-014-0172-4 [cited 2022 June 24]
24. Sahoo S, Mehra A, Grover S. Acute Hyperglycemia Associated with Psychotic Symptoms in a Patient with Type 1 Diabetes Mellitus: A Case Report. Innov Clin Neurosci. 2016;13(11-12):25-27. Published 2016 Dec 1. [cited 2022 June 24]
25. Psyche Rights Website New York Times Series [cited 2021 Aug 4]
26. Dyer O. Lilly investigated in US over the marketing of olanzapine. BMJ. 2007;334(7586):171. doi:10.1136/bmj.39105.427731.DB [cited 2022 June 24]
27. “Is There A Connection between Food Allergies and Mental Health?” published by Integrative Psychiatry [online] [cited 2022 June 24]
28. Głąbska D, Guzek D, Groele B, Gutkowska K. Fruit and Vegetable Intake and Mental Health in Adults: A Systematic Review. Nutrients. 2020;12(1):115. Published 2020 Jan 1. doi:10.3390/nu12010115 [cited 2022 June 24]
29. Dickerson F, Stallings C, Origoni A, Vaughan C, Khushalani S, Yolken R. Markers of gluten sensitivity in acute mania: a longitudinal study. Psychiatry Res. 2012 Mar 30;196(1):68-71. doi: 10.1016/j.psychres.2011.11.007. Epub 2012 Mar 3. PMID: 22386570. [cited 2022 June 24]
30. Beyond The Gut: The Relationship Between Gluten, Psychosis, And Schizophrenia May 16, 2018 by James Greenblatt, MD & Desiree Delane, MS [cited 2022 June 24]
31. Boston University publication, “Adaptation and implementation of Open Dialogue in the United States.” published 2017 [cited 2022 June 24]
32. Samaroo D, Dickerson F, Kasarda DD, et al. Novel immune response to gluten in individuals with schizophrenia.Schizophr Res. 2010;118(1-3):248-255. doi:10.1016/j.schres.2009.08.009 [cited 2022 June 24]
33. Kraeuter AK, Phillips R, Sarnyai Z. The Gut Microbiome in Psychosis From Mice to Men: A Systematic Review of Preclinical and Clinical Studies. Front Psychiatry. 2020;11:799. Published 2020 Aug 11. doi:10.3389/fpsyt.2020.00799 [cited 2022 June 24]
34. Tanya T. Nguyen, Hugh Hathaway, Tomasz Kosciolek, Rob Knight, Dilip V. Jeste, Gut microbiome in serious mental illnesses: A systematic review and critical evaluation, Schizophrenia Research, 2019, Aug 26, ISSN 0920-9964 [cited 2022 June 24]
35. Emily G. Severance, Robert H. Yolken, William W. Eaton, Autoimmune diseases, gastrointestinal disorders and the microbiome in schizophrenia: more than a gut feeling, Schizophrenia Research, Volume 176, Issue 1, 2016, Pages 23-35, ISSN 0920-9964, [cited 2022 June 24]
36. Khalil RM, Khedr NF. Curcumin Protects against Monosodium Glutamate Neurotoxicity and Decreasing NMDA2B and mGluR5 Expression in Rat Hippocampus. Neurosignals. 2016;24(1):81-87. doi: 10.1159/000442614. Epub 2016 Aug 17. PMID: 27529496. [cited 2022 June 24]
37. Padder T, Udyawar A , Azhar N, Jaghab K, Acute Hypoglycemia Presenting as Acute Psychosis Department of Psychiatry, Nassau University Medical Center [First Published December 2005]. [cited 2022 June 24]
38. Brady WJ Jr, Duncan CW. Hypoglycemia masquerading as acute psychosis and acute cocaine intoxication. Am J Emerg Med. 1999 May;17(3):318-9. doi: 10.1016/s0735-6757(99)90140-7. PMID: 10337905. [cited 2022 June 24]
39. Leonardo Tondo, Nereide Rudas, The course of a seasonal bipolar disorder influenced by caffeine, Journal of Affective Disorders, Volume 22, Issue 4, 1991, Pages 249-251. cited 2022 June 24]
40. T. S. Sathyanarayana Rao, M. R. Asha, B. N. Ramesh, and K. S. Jagannatha Rao Understanding nutrition, depression and mental illnesses Indian J Psychiatry. 2008 Apr-Jun; 50(2): 77–82. [cited 2022 June 24]
41. van der Heijden, F., Fekkes, D., Tuinier, S. et al. Amino acids in schizophrenia: evidence for lower tryptophan availability during treatment with atypical antipsychotics?. J Neural Transm 112, 577–585 (2005). [cited 2022 June 24]
42. Zisapel N. New perspectives on the role of melatonin in human sleep, circadian rhythms and their regulation. Br J Pharmacol. 2018;175(16):3190-3199. doi:10.1111/bph.14116 [cited 2022 June 24]
43. McNamara R K, “Mitigation of Inflammation-Induced Mood Dysregulation by Long-Chain Omega-3 Fatty Acids.” Journal of American College of Nutrition 2015;34 Suppl 1(0 1):48-55. DOI: 10.1080/07315724.2015.1080527 [cited 2022 June 24]
44. Malcolm Peet, Eicosapentaenoic acid in the treatment of schizophrenia and depression: rationale and preliminary double-blind clinical trial results, Prostaglandins, Leukotrienes and Essential Fatty Acids, Volume 69, Issue 6, 2003, Pages 477-485. [cited 2022 June 24]
45. “Trace elements in human health.” book and PDF authored and published 1996 by the World Health Org, [published online] [cited 2022 June 24]
46. LOW-DOSE LITHIUM: AN EFFECTIVE TREATMENT FOR MOOD DISORDERS Naturopathic Doctor News and Review by Tolle Causam Nicole Cain, ND, MA. [Published 2020 Mar 2] [cited 2022 June 24]
47. H.E. Sartori, Lithium orotate in the treatment of alcoholism and related conditions, Alcohol, Volume 3, Issue 2, 1986, Pages 97-100, ISSN 0741-8329. [cited 2022 June 24]
48. Lakhan SE, Vieira KF. Nutritional therapies for mental disorders. Nutr J. 2008;7:2. Published 2008 Jan 21. doi:10.1186/1475-2891-7-2 [cited 2022 June 24]
49. “Understanding the Differences Between Lithium and Lithium Orotate,” Amen Clinics, December 17, 2019 By Melissa Quinn, MD. [cited 2022 June 24]
50. Kling MA, Manowitz P, Pollack IW. Rat brain and serum lithium concentrations after acute injections of lithium carbonate and orotate. J Pharm Pharmacol. 1978 Jun;30(6):368-70. doi: 10.1111/j.2042-7158.1978.tb13258.x. PMID: 26768. [cited 2022 June 24]
51. Sher L. Suicide in men. J Clin Psychiatry. 2015 Mar;76(3):e371-2. doi: 10.4088/JCP.14com09554. PMID: 25830461. [cited 2022 June 24]
52. Schrauzer, G.N., Shrestha, K.P. Lithium in drinking water and the incidences of crimes, suicides, and arrests related to drug addictions. Biol Trace Elem Res 25, 105–113 (1990). [cited 2022 June 24]
53. Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis BMJ 2013; 346 (Published 27 June 2013) Andrea Cipriani, lecturer in psychiatry, Keith Hawton, professor of psychiatry, Sarah Stockton, senior information scientist, John R Geddes, professor of epidemiological psychiatry. [cited 2022 June 24]
54. Hoffer A, Osmond H. TREATMENT OF SCHIZOPHRENIA WITH NICOTINIC ACID. A TEN YEAR FOLLOW-UP. Acta Psychiatr Scand. 1964;40(2):171-89. doi: 10.1111/j.1600-0447.1964.tb05744.x. PMID: 14235254. [cited 2022 June 24]
55. Orthomolecular Treatment of Orthomolecular Schizophrenia Association of Great Britain; London, England, September 28-30, 1971. A. Hoffer, M.D., Ph.D., F.A.P.A. [cited 2022 June 24]
56. Arinola G, Idonije B, Akinlade K, Ihenyen O. Essential trace metals and heavy metals in newly diagnosed schizophrenic patients and those on anti-psychotic medication. J Res Med Sci. 2010;15(5):245-249. [cited 2022 June 24]
57. Journal of Neurology, Neurosurgery, and Psychiatry, 1974, 37, 954-958 Psychiatric aspects of methylmercury poisoning H. I. MAGHAZAJI From the Department of Medicine, Medical College, Baghdad University, Baghdad, Iraq [cited 2022 June 24]
58. Aschner, M., Walker, S. The neuropathogenesis of mercury toxicity. Mol Psychiatry 7, S40–S41 (2002). [cited 2022 June 24]
59. The American Journal of Psychiatry Mercury Poisoning: A Case of a Complex Neuropsychiatric Illness Xuebing Huang, M.D. Samuel Law, M.D., F.R.C.P.C. Dan Li, M.D. Xin Yu, M.D. Bing Li, M.D. [cited 2022 June 24]
60. Environmental Exposures and Depression: Biological Mechanisms and Epidemiological Evidence Annual Review of Public Health Vol. 40:239-259 (Volume publication date April 2019) First published as a Review in Advance on 2019 Jan 11 [cited 2022 June 24]
61. Collaborative on Mental Health and the Environment Mental Health and Environmental Exposures from the Learning and Developmental Disabilities Initiative, November 2008. [cited 2022 June 24]
62. Mittal VA, Vargas T, Osborne KJ, et al. Exercise Treatments for Psychosis: A Review. Curr Treat Options Psychiatry. 2017;4(2):152-166. doi:10.1007/s40501-017-0112-2. [cited 2022 June 24]
63. Mead MN. Benefits of sunlight: a bright spot for human health [published correction appears in Environ Health Perspect. 2008 May;116(5):A197]. Environ Health Perspect. 2008;116(4):A160-A167. doi:10.1289/ehp.116-a160 [cited 2022 June 24]
64. Siebern AT, Suh S, Nowakowski S. Non-pharmacological treatment of insomnia. Neurotherapeutics. 2012;9(4):717-727. doi:10.1007/s13311-012-0142-9 [cited 2022 June 24]
65. Cannabis-Induced Psychosis: A Review Psychiatric Times, Vol 34 No 7, Volume 34, Issue 7July 14, 2017 Ruby S. Grewal, MD, Tony P. George, MD, FRCPC. [cited 2022 June 24]
66. Arendt M, Rosenberg R, Foldager L, Perto G, Munk-Jørgensen P. Cannabis-induced psychosis and subsequent schizophrenia-spectrum disorders: follow-up study of 535 incident cases. Br J Psychiatry. 2005 Dec;187:510-5. doi: 10.1192/bjp.187.6.510. PMID: 16319402. [cited 2022 June 24]
67. Rottanburg D, Robins AH, Ben-Arie O, Teggin A, Elk R. Cannabis-associated psychosis with hypomanic features Lancet. 1982 Dec 18;2(8312):1364-6. doi: 10.1016/s0140-6736(82)91270-3. PMID: 6129463. [cited 2022 June 24]
68. Morrison AK. Cognitive behavior therapy for people with schizophrenia. Psychiatry (Edgmont). 2009;6(12):32-39. [cited 2022 June 24]
69. Freeman et al., “Open Dialogue: A Review of the Evidence.” published in Psychiatryonline 18 Oct 2018 [cited 2022 June 24]
70. Wilson G, Farrell D, Barron I, Hutchins J, Whybrow D, Kiernan MD. The Use of Eye-Movement Desensitization Reprocessing (EMDR) Therapy in Treating Post-traumatic Stress Disorder-A Systematic Narrative Review. Front Psychol. 2018;9:923. Published 2018 Jun 6. doi:10.3389/fpsyg.2018.00923 [cited 2022 June 24]
71. Frueh BC, Grubaugh AL, Cusack KJ, Kimble MO, Elhai JD, Knapp RG. Exposure-based cognitive-behavioral treatment of PTSD in adults with schizophrenia or schizoaffective disorder: a pilot study. J Anxiety Disord. 2009;23(5):665-675. doi:10.1016/j.janxdis.2009.02.005 [cited 2022 June 24]
72. David D, Cristea I, Hofmann SG. Why Cognitive Behavioral Therapy Is the Current Gold Standard of Psychotherapy. Front Psychiatry. 2018;9:4. Published 2018 Jan 29. doi:10.3389/fpsyt.2018.00004 [cited 2022 June 24]
73. Clapp M, Aurora N, Herrera L, Bhatia M, Wilen E, Wakefield S. Gut microbiota’s effect on mental health: The gut-brain axis. Clin Pract. 2017;7(4):987. Published 2017 Sep 15. doi:10.4081/cp.2017.987 [cited 2022 June 24]
74. Bonaz B, Bazin T, Pellissier S. The Vagus Nerve at the Interface of the Microbiota-Gut-Brain Axis. Front Neurosci. 2018 Feb 7;12:49. doi: 10.3389/fnins.2018.00049. PMID: 29467611; PMCID: PMC5808284. [cited 2022 June 24]
75. Ronald Walker, John R. Lupien, The Safety Evaluation of Monosodium Glutamate, The Journal of Nutrition, Volume 130, Issue 4, April 2000, Pages 1049S–1052S [cited 2022 June 24]
76. Young SN. The effect of raising and lowering tryptophan levels on human mood and social behaviour. Philos Trans R Soc Lond B Biol Sci. 2013;368(1615):20110375. Published 2013 Feb 25. doi:10.1098/rstb.2011.0375 [cited 2022 June 24]
77. Zhang, J., Ma, L., Chang, L.et al. A key role of the subdiaphragmatic vagus nerve in the depression-like phenotype and abnormal composition of gut microbiota in mice after lipopolysaccharide administration. Transl Psychiatry 10, 186 (2020). https://doi.org/10.1038/s41398-020-00878-3 [cited 2022 June 24]
78. McAllister-Williams, R.H., Sousa, S., Kumar, A. et al. The effects of vagus nerve stimulation on the course and outcomes of patients with bipolar disorder in a treatment-resistant depressive episode: a 5-year prospective registry. Int J Bipolar Disord8,13 (2020). https://doi.org/10.1186/s40345-020-0178-4 [cited 2022 June 24]
79. Breit S, Kupferberg A, Rogler G, Hasler G. Vagus Nerve as Modulator of the Brain-Gut Axis in Psychiatric and Inflammatory Disorders. Front Psychiatry. 2018;9:44. Published 2018 Mar 13. doi:10.3389/fpsyt.2018.00044 [cited 2022 June 24]
80. NIH Office of Dietary Supplements, “Omega-3 Fatty Acids – Health Professional Fact Sheet.” Oct 1, 2020 [cited 2022 June 24]
81. Christensen O, Christensen E, Fat consumption and schizophrenia Acta Psychiatrica Scandinavica [published: November 1988]. [cited 2022 June 24]
82. Aucoin M, LaChance L, Cooley K, Kidd S. Diet and Psychosis: A Scoping Review. Neuropsychobiology. 2020;79(1):20-42. doi: 10.1159/000493399. Epub 2018 Oct 25. PMID: 30359969. [cited 2022 June 24]

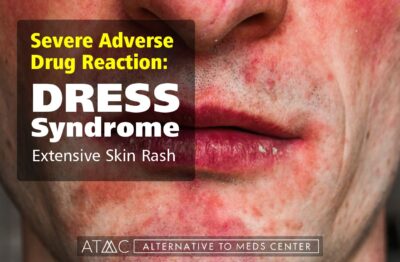 Doctors also prescribe Zyprexa when other drugs do not work, such as when persons with depression do not respond to antidepressants. So, some Zyprexa users are already taking it because previous drug treatments were unsatisfactory. Studies clearly show that a drug like Zyprexa can produce no improvements for some, and horrible outcomes for others. These can include obstruction or paralysis of the intestines that can lead to sepsis and death.2
Doctors also prescribe Zyprexa when other drugs do not work, such as when persons with depression do not respond to antidepressants. So, some Zyprexa users are already taking it because previous drug treatments were unsatisfactory. Studies clearly show that a drug like Zyprexa can produce no improvements for some, and horrible outcomes for others. These can include obstruction or paralysis of the intestines that can lead to sepsis and death.2 Cognitive Behavioral Therapy, other forms of psychotherapy 10,68,70,71
Cognitive Behavioral Therapy, other forms of psychotherapy 10,68,70,71 According to Health Quality Ontario, a 2018 review found that individuals fared better with CBT when compared to medication alone. Patients experienced a reduction in “positive” or active symptoms of psychosis, which participants reported as a desirable treatment outcome. We also learn from a 2009 study published in Psychiatry that CBT proved effective for persons who did not respond well to medication. Such studies expressed a need for more research into CBT and other effective and viable treatment options over medication alone.10,61,68,72
According to Health Quality Ontario, a 2018 review found that individuals fared better with CBT when compared to medication alone. Patients experienced a reduction in “positive” or active symptoms of psychosis, which participants reported as a desirable treatment outcome. We also learn from a 2009 study published in Psychiatry that CBT proved effective for persons who did not respond well to medication. Such studies expressed a need for more research into CBT and other effective and viable treatment options over medication alone.10,61,68,72 Better dietary choices are seen as helpful in a vast array of symptoms such as mood swings, psychosis, depression, and others.33,34,35,48
Better dietary choices are seen as helpful in a vast array of symptoms such as mood swings, psychosis, depression, and others.33,34,35,48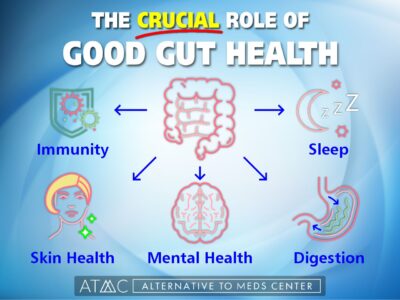 The “gut-brain axis” has come to the forefront of nutritional therapies for mental health. A healthy microbiome is essential to monitoring thousands of factors in human health, including those that support mental health, as suggested in a 2016 Schizophrenia Research study by Severance et al. According to a review of clinical data, there is a strong link between gut inflammation and symptoms of schizophrenia. Other studies published in Science Direct suggest a promising avenue for the treatment of schizophrenia may be further developed by closely monitoring and comparing microbiota of non-schizophrenic and schizophrenic patients.33,34,35,73,74,79
The “gut-brain axis” has come to the forefront of nutritional therapies for mental health. A healthy microbiome is essential to monitoring thousands of factors in human health, including those that support mental health, as suggested in a 2016 Schizophrenia Research study by Severance et al. According to a review of clinical data, there is a strong link between gut inflammation and symptoms of schizophrenia. Other studies published in Science Direct suggest a promising avenue for the treatment of schizophrenia may be further developed by closely monitoring and comparing microbiota of non-schizophrenic and schizophrenic patients.33,34,35,73,74,79 Massage therapy can help,7 but likely won’t adequately replace the need for antipsychotic medication in the middle of a full-blown crisis situation. Over time, however, individuals with depression, schizophrenia, or bipolar disorder, can begin combining simple therapies for effective relief and improvement.
Massage therapy can help,7 but likely won’t adequately replace the need for antipsychotic medication in the middle of a full-blown crisis situation. Over time, however, individuals with depression, schizophrenia, or bipolar disorder, can begin combining simple therapies for effective relief and improvement. Alternative to Meds Center uses a comprehensive array of
Alternative to Meds Center uses a comprehensive array of