1. Kim EJ, Lim SY, Lee HJ, Lee JY, Choi S, Kim SY, Kim JM, Shin IS, Yoon JS, Yang SJ, Kim SW. Low dietary intake of n-3 fatty acids, niacin, folate, and vitamin C in Korean patients with schizophrenia and the development of dietary guidelines for schizophrenia. Nutr Res. 2017 Sep;45:10-18. doi: 10.1016/j.nutres.2017.07.001. Epub 2017 Jul 19. PMID: 29037327. [cited 2022 June 21]
2. Głąbska D, Guzek D, Groele B, Gutkowska K. Fruit and Vegetable Intake and Mental Health in Adults: A Systematic Review. Nutrients. 2020;12(1):115. Published 2020 Jan 1. doi:10.3390/nu12010115 [cited 2022 June 21]
3. Michalsen A, et al., “Rapid stress reduction and anxiolysis among distressed women as a consequence of a 3-month intensive yoga program.” A Controlled Clinical Trial in Medical Science Monitor [PMID 16319785 ] 2005 Dec 11 [cited 2022 June 21]
4. Sharma A, Madaan V, Petty FD. Exercise for mental health. Prim Care Companion J Clin Psychiatry. 2006;8(2):106. doi:10.4088/pcc.v08n0208a [cited 2022 June 21]
5. Callaghan P, “Exercise: A neglected intervention in mental health care.” J Psychiatr Ment Health Nurs [PMID 15255923] 2004 Aug 11 [cited 2022 June 21]
6. Neale G, Hogan H, Sevdalis N. Misdiagnosis: analysis based on case record review with proposals aimed to improve diagnostic processes. Clin Med (Lond). 2011;11(4):317-321. doi:10.7861/clinmedicine.11-4-317 [cited 2022 June 21]
7. FDA Access Data LAMICTAL label [cited 2022 June 21]
8. Suppes T, Marangell LB, Bernstein IH, et al. A single blind comparison of lithium and lamotrigine for the treatment of bipolar II depression. J Affect Disord. 2008;111(2-3):334-343. doi:10.1016/j.jad.2008.02.004 [cited 2022 June 21]
9. Kråkvik B, Gråwe RW, Hagen R, Stiles TC. Cognitive behaviour therapy for psychotic symptoms: a randomized controlled effectiveness trial. Behav Cogn Psychother. 2013;41(5):511-524. doi:10.1017/S1352465813000258 [cited 2022 June 21]
10. Seikkula J, Olson ME. The open dialogue approach to acute psychosis: its poetics and micropolitics. Fam Process. 2003 Fall;42(3):403-18. doi: 10.1111/j.1545-5300.2003.00403.x. PMID: 14606203. [cited 2022 June 21]
11. Mor N, Haran D. Cognitive-behavioral therapy for depression. Isr J Psychiatry Relat Sci. 2009;46(4):269-73. PMID: 20635774. [cited 2022 June 21]
12. Health Quality Ontario . Cognitive Behavioural Therapy for Psychosis: A Health Technology Assessment. Ont Health Technol Assess Ser. 2018;18(5):1-141. Published 2018 Oct 24. [cited 2022 June 21]
13. Sudak DM. Cognitive behavioral therapy for depression. Psychiatr Clin North Am. 2012 Mar;35(1):99-110. doi: 10.1016/j.psc.2011.10.001. Epub 2011 Dec 3. PMID: 22370493. [cited 2022 June 21]
14. van den Berg DP, de Bont PA, van der Vleugel BM, de Roos C, de Jongh A, Van Minnen A, van der Gaag M. Prolonged exposure vs eye movement desensitization and reprocessing vs waiting list for posttraumatic stress disorder in patients with a psychotic disorder: a randomized clinical trial. JAMA Psychiatry. 2015 Mar;72(3):259-67. doi: 10.1001/jamapsychiatry.2014.2637. PMID: 25607833. [cited 2022 June 21]
15. APA Div 12, Society of Clinical Psychology, “What is Exposure Therapy?” Clinical Practice Guidelines, [Internet] 2017 Jul [cited 2022 June 21]
16. Amminger, Schafer, Papageorgiou, Klier, Cotton, Harrigan, MacKinnon, McGorry, Berger, “Long-chain omega-3 fatty acids for indicated prevention of psychotic disorders: a randomized, placebo-controlled trial” US National Library of Medicine [Internet] 2010 Feb [cited 2022 June 21]
17. Firth J, Gangwisch JE, Borisini A, Wootton RE, Mayer EA. Food and mood: how do diet and nutrition affect mental wellbeing? [published correction appears in BMJ. 2020 Nov 9;371:m4269]. BMJ. 2020;369:m2382. Published 2020 Jun 29. doi:10.1136/bmj.m2382 [cited 2022 June 21]
18. Plitman E, Nakajima S, de la Fuente-Sandoval C, et al. Glutamate-mediated excitotoxicity in schizophrenia: a review. Eur Neuropsychopharmacol. 2014;24(10):1591-1605. doi:10.1016/j.euroneuro.2014.07.015. [cited 2022 June 21]
19. Leonardo Tondo, Nereide Rudas, The course of a seasonal bipolar disorder influenced by caffeine, Journal of Affective Disorders, Volume 22, Issue 4, 1991, Pages 249-251. [cited 2022 June 21]
20. van der Heijden, F., Fekkes, D., Tuinier, S. et al. Amino acids in schizophrenia: evidence for lower tryptophan availability during treatment with atypical antipsychotics?. J Neural Transm 112, 577–585 (2005). [cited 2022 June 21]
21. Environmental Exposures and Depression: Biological Mechanisms and Epidemiological Evidence Annual Review of Public Health Vol. 40:239-259 (Volume publication date April 2019) First published as a Review in Advance on 2019 Jan 11 [cited 2022 June 21]
22. Collaborative on Mental Health and the Environment Mental Health and Environmental Exposures from the Learning and Developmental Disabilities Initiative, November 2008. [[cited 2022 June 21]
23. Understanding nutrition, depression and mental illnesses Indian J Psychiatry. 2008 Apr-Jun; 50(2): 77–82. T. S. Sathyanarayana Rao, M. R. Asha, B. N. Ramesh, and K. S. Jagannatha Rao [cited 2022 June 21]
24. Mittal VA, Vargas T, Osborne KJ, et al. Exercise Treatments for Psychosis: A Review. Curr Treat Options Psychiatry. 2017;4(2):152-166. doi:10.1007/s40501-017-0112-2.[cited 2022 June 21]
25. Lakhan SE, Vieira KF. Nutritional therapies for mental disorders. Nutr J. 2008;7:2. Published 2008 Jan 21. doi:10.1186/1475-2891-7-2 [cited 2022 June 21]
26. Hoffer A, Osmond H. TREATMENT OF SCHIZOPHRENIA WITH NICOTINIC ACID. A TEN YEAR FOLLOW-UP. Acta Psychiatr Scand. 1964;40(2):171-89. doi: 10.1111/j.1600-0447.1964.tb05744.x. PMID: 14235254. [cited 2022 June 21]
27. Malcolm Peet, Eicosapentaenoic acid in the treatment of schizophrenia and depression: rationale and preliminary double-blind clinical trial results, Prostaglandins, Leukotrienes and Essential Fatty Acids, Volume 69, Issue 6, 2003, Pages 477-485. [cited 2022 June 21]
28. Acta Psychiatrica Scandinavica Fat consumption and schizophrenia O. Christensen M.D., E. Christensen First published: November 1988. [cited 2022 June 21]
29. Acute Hypoglycemia Presenting as Acute Psychosis Tanveer Padder MD, Aparna Udyawar MD, Nouman Azhar MD, Kamil Jaghab MD From the Department of Psychiatry, Nassau University Medical Center, 2201 Hempstead Turnpike, East Meadow NY 11554 USA.First Published December 2005. [cited 2022 June 21]
30. Brady WJ Jr, Duncan CW. Hypoglycemia masquerading as acute psychosis and acute cocaine intoxication. Am J Emerg Med. 1999 May;17(3):318-9. doi: 10.1016/s0735-6757(99)90140-7. PMID: 10337905. [cited 2022 June 21]
31. Low Plasma GABA Is a Trait-Like Marker for Bipolar Illness NEUROPSYCHOPHARMACOLOGY 1993-VOL. 9, NO. 2 Frederick Petty, Ph.D., M.D., Gerald Kramer, Mark Fulton, M.D., Frederick G. Moeller, M.D., and John Rush, M.D. [cited 2021 Nov 29]
32. Lionetti E, Leonardi S, Franzonello C, Mancardi M, Ruggieri M, Catassi C. Gluten Psychosis: Confirmation of a New Clinical Entity. Nutrients. 2015 Jul 8;7(7):5532-9. doi: 10.3390/nu7075235. PMID: 26184290; PMCID: PMC4517012. [cited 2022 June 21]
33. Is There a Connection Between Food Allergies and Mental Health? Integrative Psychiatry 2012 Sep 6 [cited 2022 June 21]
34. Farina M, Aschner M, da Rocha JBT. The catecholaminergic neurotransmitter system in methylmercury-induced neurotoxicity. Adv Neurotoxicol. 2017;1:47-81. doi:10.1016/bs.ant.2017.07.002 [cited 2022 June 21]
35. Kraeuter AK, Phillips R, Sarnyai Z. The Gut Microbiome in Psychosis From Mice to Men: A Systematic Review of Preclinical and Clinical Studies. Front Psychiatry. 2020;11:799. Published 2020 Aug 11. doi:10.3389/fpsyt.2020.00799 [cited 2022 June 21]
36. Tanya T. Nguyen, Hugh Hathaway, Tomasz Kosciolek, Rob Knight, Dilip V. Jeste, Gut microbiome in serious mental illnesses: A systematic review and critical evaluation, Schizophrenia Research, 2019, Aug 26, ISSN 0920-9964 [cited 2022 June 21]
37. Emily G. Severance, Robert H. Yolken, William W. Eaton, Autoimmune diseases, gastrointestinal disorders and the microbiome in schizophrenia: more than a gut feeling, Schizophrenia Research, Volume 176, Issue 1, 2016, Pages 23-35, ISSN 0920-9964 [cited 2022 June 21]
38. Lundbeck Institute Campus Microbes and brain share neurochemistry Professor Mark Lyte (Iowa State University College of Veterinary Medicine, Iowa, USA0 Published Mar 6, 2019. [cited 2022 June 21]
39. Kirkpatrick, B., Alphs, L., & Buchanan, R. W. (1992). The concept of supersensitivity psychosis. Journal of Nervous and Mental Disease, 180(4), 265–270. [cited 2022 June 21]
40. Chouinard G, Jones BD. Neuroleptic-induced supersensitivity psychosis: clinical and pharmacologic characteristics. Am J Psychiatry. 1980 Jan;137(1):16-21 [cited 2022 June 21]
41. Prabhavalkar KS, Poovanpallil NB, Bhatt LK. Management of bipolar depression with lamotrigine: an antiepileptic mood stabilizer. Front Pharmacol. 2015;6:242. Published 2015 Oct 23. doi:10.3389/fphar.2015.00242 [cited 2022 June 21]
42. Efficacy of Equine Therapy: Mounting Evidence Edward J. Cumella Ph.D. and Sharon Simpson Jun 17, 2014. [cited 2022 June 21]
43. Craft LL, Perna FM. The Benefits of Exercise for the Clinically Depressed. Prim Care Companion J Clin Psychiatry. 2004;6(3):104-111. doi:10.4088/pcc.v06n0301. [cited 2022 June 21]
44. Romaniuk M, Evans J, Kidd C. Evaluation of an equine-assisted therapy program for veterans who identify as ‘wounded, injured or ill’ and their partners. PLoS One. 2018;13(9):e0203943. Published 2018 Sep 27. doi:10.1371/journal.pone.0203943 [cited 2022 June 21]
45. Frueh BC, Grubaugh AL, Cusack KJ, Kimble MO, Elhai JD, Knapp RG. Exposure-based cognitive-behavioral treatment of PTSD in adults with schizophrenia or schizoaffective disorder: a pilot study. J Anxiety Disord. 2009;23(5):665-675. doi:10.1016/j.janxdis.2009.02.005 [cited 2022 June 21]
46. Knüppel A, Shipley MJ, Llewellyn CH, Brunner EJ. Sugar intake from sweet food and beverages, common mental disorder and depression: prospective findings from the Whitehall II study. Sci Rep. 2017;7(1):6287. Published 2017 Jul 27. doi:10.1038/s41598-017-05649-7 [cited 2022 June 21]
47. Brown J, Introduction: An Update on Psychiatric Effects of Toxic Exposure. Psychiatric Times Sept 30 2016 Vol 33 No. 9 Volume 33 Issue 9 [cited 2022 June 21]
48. Michalsen A, Grossman P, Acil A, Langhorst J, Lüdtke R, Esch T, Stefano GB, Dobos GJ. Rapid stress reduction and anxiolysis among distressed women as a consequence of a three-month intensive yoga program. Med Sci Monit. 2005 Dec;11(12):CR555-561. Epub 2005 Nov 24. PMID: 16319785. [cited 2022 June 21]
50. Choudhary AK, Lee YY. Neurophysiological symptoms and aspartame: What is the connection? Nutr Neurosci. 2018 Jun;21(5):306-316. doi: 10.1080/1028415X.2017.1288340. Epub 2017 Feb 15. PMID: 28198207. [cited 2022 June 21]

 A low glycemic diet including organic whole foods, chemical and gluten-free 1,17
A low glycemic diet including organic whole foods, chemical and gluten-free 1,17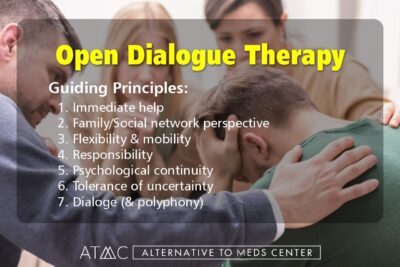 Krakvik et al’s 2013 study reported significant improvements from participating in regularly scheduled CBT sessions as a natural alternative to Lamictal or other drug-based treatment. The trend in improvements shown at one-year and two-year post-treatment follow-ups suggested to the researchers that talk therapy ought to be made available as a routine treatment in psychosis-type disorders.9
Krakvik et al’s 2013 study reported significant improvements from participating in regularly scheduled CBT sessions as a natural alternative to Lamictal or other drug-based treatment. The trend in improvements shown at one-year and two-year post-treatment follow-ups suggested to the researchers that talk therapy ought to be made available as a routine treatment in psychosis-type disorders.9 The government of Ontario Canada funded a large scope assessment on the practical benefits of adding CBT psychotherapy sessions to regular care for patients with schizophrenia and related disorders such as schizoaffective and various forms of psychosis.12 In general, participants and their family members felt positive results made CBT a welcome choice for treatment programs, especially in concert with medication management. In this way, symptoms could be well-managed and new coping skills could be learned for dealing with symptoms of psychosis so the condition was better able to be managed. CBT showed the most consistent benefits for reducing overall psychotic symptoms compared to other forms of psychotherapy in the assessment.
The government of Ontario Canada funded a large scope assessment on the practical benefits of adding CBT psychotherapy sessions to regular care for patients with schizophrenia and related disorders such as schizoaffective and various forms of psychosis.12 In general, participants and their family members felt positive results made CBT a welcome choice for treatment programs, especially in concert with medication management. In this way, symptoms could be well-managed and new coping skills could be learned for dealing with symptoms of psychosis so the condition was better able to be managed. CBT showed the most consistent benefits for reducing overall psychotic symptoms compared to other forms of psychotherapy in the assessment.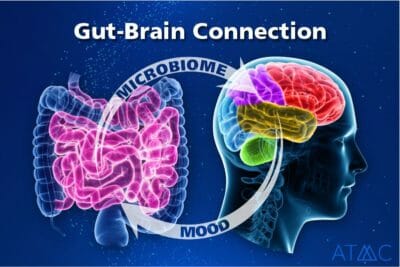 A journal article published in 2020 in the Frontiers in Psychiatry covered various correlations between psychosis and the gut microbiome. This systematic review found that the gut microbiome is fundamentally different in psychosis compared to healthy controls. The types of microbes and diversity were altered between the two groups. The researchers discuss the possibility of. manipulating the gut microbiome as a technique to improve psychiatric symptoms and even the potential development of treating schizophrenia and related psychotic disorders in a novel fashion.35 Other researchers in a systematic review of sixteen articles found that all 16 studies reported alterations in the abundance and diversity of gut microbiome in patients with severe mental impairments versus the microbiome of non-psychiatric normal controls.36 And yet another article published in Schizophrenia Research found evidence that the gut microbiota is highly involved in inflammation, gut permeability, and digestion itself, and how these altered bacterial compositions may explain inefficient gluten digestion and how inflammatory permeability in some scenarios can be a risk factor for schizophrenia.37
A journal article published in 2020 in the Frontiers in Psychiatry covered various correlations between psychosis and the gut microbiome. This systematic review found that the gut microbiome is fundamentally different in psychosis compared to healthy controls. The types of microbes and diversity were altered between the two groups. The researchers discuss the possibility of. manipulating the gut microbiome as a technique to improve psychiatric symptoms and even the potential development of treating schizophrenia and related psychotic disorders in a novel fashion.35 Other researchers in a systematic review of sixteen articles found that all 16 studies reported alterations in the abundance and diversity of gut microbiome in patients with severe mental impairments versus the microbiome of non-psychiatric normal controls.36 And yet another article published in Schizophrenia Research found evidence that the gut microbiota is highly involved in inflammation, gut permeability, and digestion itself, and how these altered bacterial compositions may explain inefficient gluten digestion and how inflammatory permeability in some scenarios can be a risk factor for schizophrenia.37 There are considerable advantages of designing an improved diet in treating mental health issues including epilepsy, schizophrenia, psychosis, and other disorders.2 For more than 100 years, physicians have recommended diet modifications with successful outcomes in the treatment and management of these types of mental health issues.1 Adopting a whole food diet is extremely helpful, as well as eliminating sugar, caffeine, and chemical-laden processed food. A focus on maintaining a healthy microbiome has also received much positive attention in research and clinical practice, especially in helping persons with psychosis, schizoaffective disorder, Lamictal side effects, or similar conditions.35,36,37,46
There are considerable advantages of designing an improved diet in treating mental health issues including epilepsy, schizophrenia, psychosis, and other disorders.2 For more than 100 years, physicians have recommended diet modifications with successful outcomes in the treatment and management of these types of mental health issues.1 Adopting a whole food diet is extremely helpful, as well as eliminating sugar, caffeine, and chemical-laden processed food. A focus on maintaining a healthy microbiome has also received much positive attention in research and clinical practice, especially in helping persons with psychosis, schizoaffective disorder, Lamictal side effects, or similar conditions.35,36,37,46 Using natural Lamictal alternatives can be blended into a person’s regimen with great advantages. One common problem when one stops taking Lamictal abruptly is that there has likely been an adaptation to the drug.39 If Lamictal was holding back Calcium gated channels, dopamine, glutamate, or aspartate,41 and suddenly you take the drug away, there can be an over-excitability as those stimulatory chemicals will now be rushing in and the receptors for them have likely upregulated.40 Lamictal holds back these neurochemicals and the receptors can become highly receptive due to the absence.40 After removing the drug, there is a more normal amount of neurochemicals available activating receptors that were basically starving. The excitatory excess can then cause the person to appear as if they are having another psychotic event when it would really be better framed as a neuroadaptive medication withdrawal reaction. When a
Using natural Lamictal alternatives can be blended into a person’s regimen with great advantages. One common problem when one stops taking Lamictal abruptly is that there has likely been an adaptation to the drug.39 If Lamictal was holding back Calcium gated channels, dopamine, glutamate, or aspartate,41 and suddenly you take the drug away, there can be an over-excitability as those stimulatory chemicals will now be rushing in and the receptors for them have likely upregulated.40 Lamictal holds back these neurochemicals and the receptors can become highly receptive due to the absence.40 After removing the drug, there is a more normal amount of neurochemicals available activating receptors that were basically starving. The excitatory excess can then cause the person to appear as if they are having another psychotic event when it would really be better framed as a neuroadaptive medication withdrawal reaction. When a  An often overlooked intervention in mental health crises is the effectiveness of mild forms of exercise.43 Sitting stationary or lying in bed for lengthy periods of time may be needed at times. Other gentle limbic connections, such as
An often overlooked intervention in mental health crises is the effectiveness of mild forms of exercise.43 Sitting stationary or lying in bed for lengthy periods of time may be needed at times. Other gentle limbic connections, such as