1. Sun H et al., “Effects of Electroacupuncture on Depression and the Production of Glial Cell Line-Derived Neurotrophic Factor Compared with Fluoxetine – A Randomized Controlled Pilot Study.” Journal of Alternative and Complementary Medicine [Internet] 2013 Sep PMID 23647408 [cited 2021 Feb 2]
2. Vita A et al, “The Effect of Antipsychotic Treatment on Cortical Gray Matter Changes in Schizophrenia.” Biological Psychiatry Journal of Psychiatric Neuroscience and Therapeutics Archival Report 2015 September [Internet] from Volume 78 Issue 6, P403-412 [cited 2021 Feb 2]
3. Lynch S, “Tolerance and Resistance to Drugs.” from Merck’s consumer manual, Reviewed 2019 August [cited 2021 Feb 2]
4. Waters F et al., “Severe Sleep Deprivation Causes Hallucinations and a Gradual Progression Toward Psychosis With Increasing Time Awake.” Frontiers in Psychiatry PMID30042701 [Internet[ 2018 Jul10 [cited 2021 Feb 2]
5. Horowitz M, Murray R, Taylor D, “Tapering Antipsychotic Treatment.” JAMA Psychiatry 2020 Aug 5 [Internet] [cited 2021 Feb 2]
6. Jenkins TA, Nguyen JC, Polglaze KE, Bertrand PP. Influence of Tryptophan and Serotonin on Mood and Cognition with a Possible Role of the Gut-Brain Axis. Nutrients. 2016;8(1):56. Published 2016 Jan 20. doi:10.3390/nu8010056 [cited 2021 Feb 2]
7. Ganesh S, Cortes-Briones J, Ranganathan M, Radhakrishnan R, Skosnik PD, D’Souza DC. Psychosis-Relevant Effects of Intravenous Delta-9-Tetrahydrocannabinol: A Mega Analysis of Individual Participant-Data from Human Laboratory Studies. Int J Neuropsychopharmacol. 2020 Dec 3;23(9):559-570. doi: 10.1093/ijnp/pyaa031. PMID: 32385508; PMCID: PMC7710917. [cited 2021 Feb 2]
8. Engen PA, Green SJ, Voigt RM, Forsyth CB, Keshavarzian A. The Gastrointestinal Microbiome: Alcohol Effects on the Composition of Intestinal Microbiota. Alcohol Res. 2015;37(2):223-36. PMID: 26695747; PMCID: PMC4590619.[cited 2021 Feb 2]
9. Lara DR. Caffeine, mental health, and psychiatric disorders. J Alzheimers Dis. 2010;20 Suppl 1:S239-48. doi: 10.3233/JAD-2010-1378. PMID: 20164571. [cited Feb 2]
10. “Vitamins: Their Function and Source” Fact Sheet published by Government of BC Health Link [online] [cited 2021 Feb 2]
11. Freeman et al., “Open Dialogue: A Review of the Evidence.” published in Psychiatryonline 18 Oct 2018 [cited 2021 Feb 2]
12. Morrison AK. Cognitive behavior therapy for people with schizophrenia. Psychiatry (Edgmont). 2009;6(12):32-39. [cited 2021 Feb 2]
13. Wilson G, Farrell D, Barron I, Hutchins J, Whybrow D, Kiernan MD. The Use of Eye-Movement Desensitization Reprocessing (EMDR) Therapy in Treating Post-traumatic Stress Disorder-A Systematic Narrative Review. Front Psychol. 2018;9:923. Published 2018 Jun 6. doi:10.3389/fpsyg.2018.00923 [cited 2021 Feb 2]
14. Frueh BC, Grubaugh AL, Cusack KJ, Kimble MO, Elhai JD, Knapp RG. Exposure-based cognitive-behavioral treatment of PTSD in adults with schizophrenia or schizoaffective disorder: a pilot study. J Anxiety Disord. 2009;23(5):665-675. doi:10.1016/j.janxdis.2009.02.005 [cited 2021 Feb 2]
15. David D, Cristea I, Hofmann SG. Why Cognitive Behavioral Therapy Is the Current Gold Standard of Psychotherapy. Front Psychiatry. 2018;9:4. Published 2018 Jan 29. doi:10.3389/fpsyt.2018.00004 [cited 2021 Feb 2]
16. Aucoin M, LaChance L, Clouthier SN, Cooley K. Dietary modification in the treatment of schizophrenia spectrum disorders: A systematic review. World J Psychiatry. 2020 Aug 19;10(8):187-201. doi: 10.5498/wjp.v10.i8.187. PMID: 32874956; PMCID: PMC7439299. [cited 2021 Aug 4]
17. Aucoin M, LaChance L, Cooley K, Kidd S. Diet and Psychosis: A Scoping Review. Neuropsychobiology. 2020;79(1):20-42. doi: 10.1159/000493399. Epub 2018 Oct 25. PMID: 30359969.[cited 2021 Feb 2]
18. Beyond The Gut: The Relationship Between Gluten, Psychosis, And Schizophrenia May 16, 2018 by James Greenblatt, MD & Desiree Delane, MS [cited 2021 Feb 2]
19. Lakhan SE, Vieira KF. Nutritional therapies for mental disorders. Nutr J. 2008;7:2. Published 2008 Jan 21. doi:10.1186/1475-2891-7-2 [cited 2021 Feb 2]
20. Hidese S, Nogawa S, Saito K, Kunugi H. Food allergy is associated with depression and psychological distress: A web-based study in 11,876 Japanese. J Affect Disord. 2019 Feb 15;245:213-218. doi: 10.1016/j.jad.2018.10.119. Epub 2018 Oct 26. PMID: 30408639. [cited 2021 Feb 2]
21. Dickerson F, Stallings C, Origoni A, Vaughan C, Khushalani S, Yolken R. Markers of gluten sensitivity in acute mania: a longitudinal study. Psychiatry Res. 2012 Mar 30;196(1):68-71. doi: 10.1016/j.psychres.2011.11.007. Epub 2012 Mar 3. PMID: 22386570. [cited 2021 Feb 2]
22. Kraeuter AK, Phillips R, Sarnyai Z. The Gut Microbiome in Psychosis From Mice to Men: A Systematic Review of Preclinical and Clinical Studies. Front Psychiatry. 2020;11:799. Published 2020 Aug 11. doi:10.3389/fpsyt.2020.00799 [cited 2021 Feb 2]
23. Tanya T. Nguyen, Hugh Hathaway, Tomasz Kosciolek, Rob Knight, Dilip V. Jeste, Gut microbiome in serious mental illnesses: A systematic review and critical evaluation, Schizophrenia Research, 2019, Aug 26, ISSN 0920-9964 [cited 2021 Feb 2]
24. Emily G. Severance, Robert H. Yolken, William W. Eaton, Autoimmune diseases, gastrointestinal disorders and the microbiome in schizophrenia: more than a gut feeling, Schizophrenia Research, Volume 176, Issue 1, 2016, Pages 23-35, ISSN 0920-9964, [cited 2021 Feb 2]
25. Clapp M, Aurora N, Herrera L, Bhatia M, Wilen E, Wakefield S. Gut microbiota’s effect on mental health: The gut-brain axis. Clin Pract. 2017;7(4):987. Published 2017 Sep 15. doi:10.4081/cp.2017.987 [cited 2021 Feb 2]
26. Ronald Walker, John R. Lupien, The Safety Evaluation of Monosodium Glutamate, The Journal of Nutrition, Volume 130, Issue 4, April 2000, Pages 1049S–1052S [cited 2021 Feb 2]
27. Khalil RM, Khedr NF. Curcumin Protects against Monosodium Glutamate Neurotoxicity and Decreasing NMDA2B and mGluR5 Expression in Rat Hippocampus. Neurosignals. 2016;24(1):81-87. doi: 10.1159/000442614. Epub 2016 Aug 17. PMID: 27529496. [cited 2021 Feb 2]
28. Acute Hypoglycemia Presenting as Acute Psychosis Tanveer Padder MD, Aparna Udyawar MD, Nouman Azhar MD, Kamil Jaghab MD From the Department of Psychiatry, Nassau University Medical Center, 2201 Hempstead Turnpike, East Meadow NY 11554 USA.First Published December 2005. [cited 2021 Feb 2]
29. Brady WJ Jr, Duncan CW. Hypoglycemia masquerading as acute psychosis and acute cocaine intoxication. Am J Emerg Med. 1999 May;17(3):318-9. doi: 10.1016/s0735-6757(99)90140-7. PMID: 10337905. [cited 2021 Feb 2]
30. Understanding nutrition, depression and mental illnesses Indian J Psychiatry. 2008 Apr-Jun; 50(2): 77–82. T. S. Sathyanarayana Rao, M. R. Asha, B. N. Ramesh, and K. S. Jagannatha Rao [cited 2021 Feb 2]
31. van der Heijden, F., Fekkes, D., Tuinier, S. et al. Amino acids in schizophrenia: evidence for lower tryptophan availability during treatment with atypical antipsychotics?. J Neural Transm 112, 577–585 (2005). [cited 2021 Feb 2]
32. Young SN. The effect of raising and lowering tryptophan levels on human mood and social behaviour. Philos Trans R Soc Lond B Biol Sci. 2013;368(1615):20110375. Published 2013 Feb 25. doi:10.1098/rstb.2011.0375 [cited 2021 Feb 2]
33. van der Heijden, F., Fekkes, D., Tuinier, S. et al. Amino acids in schizophrenia: evidence for lower tryptophan availability during treatment with atypical antipsychotics?. J Neural Transm 112, 577–585 (2005). [cited 2021 Feb 2]
34. Acta Psychiatrica Scandinavica Fat consumption and schizophrenia O. Christensen M.D., E. Christensen First published: November 1988. [cited 2021 Feb 2]
35. McNamara R K, “Mitigation of Inflammation-Induced Mood Dysregulation by Long-Chain Omega-3 Fatty Acids.” Journal of American College of Nutrition [Internet] 2015;34 Suppl 1(0 1):48-55. DOI: 10.1080/07315724.2015.1080527 [cited 2021 Feb 2]
36. Malcolm Peet, Eicosapentaenoic acid in the treatment of schizophrenia and depression: rationale and preliminary double-blind clinical trial results, Prostaglandins, Leukotrienes and Essential Fatty Acids, Volume 69, Issue 6, 2003, Pages 477-485. [cited 2021 Feb 2]
37. LOW-DOSE LITHIUM: AN EFFECTIVE TREATMENT FOR MOOD DISORDERS Naturopathic Doctor News and Review by Tolle Causam Nicole Cain, ND, MA. Published 2020 Mar 2 [cited 2021 Feb 2]
38. “Trace elements in human health.” book and PDF authored and published 1996 by the World Health Org, [Internet] [cited 2021 Feb 2]
39. LOW-DOSE LITHIUM: AN EFFECTIVE TREATMENT FOR MOOD DISORDERS Naturopathic Doctor News and Review by Tolle Causam Nicole Cain, ND, MA. Published 2020 Mar 2 [cited 2021 Feb 2]
40. H.E. Sartori, Lithium orotate in the treatment of alcoholism and related conditions, Alcohol, Volume 3, Issue 2, 1986, Pages 97-100, ISSN 0741-8329. [cited 2021 Jan 2]
41. “Understanding the Differences Between Lithium and Lithium Orotate,” Amen Clinics, December 17, 2019 By Melissa Quinn, MD. [cited 2021 Jan 19]
42. Kling MA, Manowitz P, Pollack IW. Rat brain and serum lithium concentrations after acute injections of lithium carbonate and orotate. J Pharm Pharmacol. 1978 Jun;30(6):368-70. doi: 10.1111/j.2042-7158.1978.tb13258.x. PMID: 26768. [cited 2021 Jan 19]
43. Schrauzer, G.N., Shrestha, K.P. Lithium in drinking water and the incidences of crimes, suicides, and arrests related to drug addictions. Biol Trace Elem Res 25, 105–113 (1990). [cited 2021 Feb 2]
44. Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis BMJ 2013; 346 (Published 27 June 2013) Andrea Cipriani, lecturer in psychiatry, Keith Hawton, professor of psychiatry, Sarah Stockton, senior information scientist, John R Geddes, professor of epidemiological psychiatry. [cited 2021 Feb 2]
45. Hoffer A, Osmond H. TREATMENT OF SCHIZOPHRENIA WITH NICOTINIC ACID. A TEN YEAR FOLLOW-UP. Acta Psychiatr Scand. 1964;40(2):171-89. doi: 10.1111/j.1600-0447.1964.tb05744.x. PMID: 14235254. [cited 2021 Feb 2]
46. Orthomolecular Treatment of Orthomolecular Schizophrenia Association of Great Britain; London, England, September 28-30, 1971. A. Hoffer, M.D., Ph.D., F.A.P.A. [cited 2021 Feb 2]
47. Arinola G, Idonije B, Akinlade K, Ihenyen O. Essential trace metals and heavy metals in newly diagnosed schizophrenic patients and those on anti-psychotic medication. J Res Med Sci. 2010;15(5):245-249. [cited 2021 Feb 2]
48. Journal of Neurology, Neurosurgery, and Psychiatry, 1974, 37, 954-958 Psychiatric aspects of methylmercury poisoning H. I. MAGHAZAJI From the Department of Medicine, Medical College, Baghdad University, Baghdad, Iraq [cited 2021 Feb 2]
49. Aschner, M., Walker, S. The neuropathogenesis of mercury toxicity. Mol Psychiatry 7, S40–S41 (2002).[cited 2021 Feb 2]
50. The American Journal of Psychiatry Mercury Poisoning: A Case of a Complex Neuropsychiatric Illness Xuebing Huang, M.D. Samuel Law, M.D., F.R.C.P.C. Dan Li, M.D. Xin Yu, M.D. Bing Li, M.D.[cited 2021 Feb 2]
51. Environmental Exposures and Depression: Biological Mechanisms and Epidemiological Evidence Annual Review of Public Health Vol. 40:239-259 (Volume publication date April 2019) First published as a Review in Advance on 2019 Jan 11 [cited 2021 Feb 2]
52. Collaborative on Mental Health and the Environment Mental Health and Environmental Exposures from the Learning and Developmental Disabilities Initiative, November 2008. [cited 2021 Feb 2]
53. Mittal VA, Vargas T, Osborne KJ, et al. Exercise Treatments for Psychosis: A Review. Curr Treat Options Psychiatry. 2017;4(2):152-166. doi:10.1007/s40501-017-0112-2.[cited 2021 Feb 2]
54. Mead MN. Benefits of sunlight: a bright spot for human health [published correction appears in Environ Health Perspect. 2008 May;116(5):A197]. Environ Health Perspect. 2008;116(4):A160-A167. doi:10.1289/ehp.116-a160 [cited 2021 Feb 2]
55. Siebern AT, Suh S, Nowakowski S. Non-pharmacological treatment of insomnia. Neurotherapeutics. 2012;9(4):717-727. doi:10.1007/s13311-012-0142-9 [cited 2021 Feb 2]
56. Cannabis-Induced Psychosis: A Review Psychiatric Times, Vol 34 No 7, Volume 34, Issue 7July 14, 2017 Ruby S. Grewal, MD , Tony P. George, MD, FRCPC. [cited 2021 Feb 2]
57. Arendt M, Rosenberg R, Foldager L, Perto G, Munk-Jørgensen P. Cannabis-induced psychosis and subsequent schizophrenia-spectrum disorders: follow-up study of 535 incident cases. Br J Psychiatry. 2005 Dec;187:510-5. doi: 10.1192/bjp.187.6.510. PMID: 16319402. [cited 2021 Feb 2]
58. Rottanburg D, Robins AH, Ben-Arie O, Teggin A, Elk R. Cannabis-associated psychosis with hypomanic features Lancet. 1982 Dec 18;2(8312):1364-6. doi: 10.1016/s0140-6736(82)91270-3. PMID: 6129463. [cited 2021 Feb 2]
59. Leonardo Tondo, Nereide Rudas, The course of a seasonal bipolar disorder influenced by caffeine, Journal of Affective Disorders, Volume 22, Issue 4, 1991, Pages 249-251. [cited 2021 Feb 2]
60. Bonaz B, Bazin T, Pellissier S. The Vagus Nerve at the Interface of the Microbiota-Gut-Brain Axis. Front Neurosci. 2018 Feb 7;12:49. doi: 10.3389/fnins.2018.00049. PMID: 29467611; PMCID: PMC5808284. [ cited 2021 Feb 2]
61. Engen PA, Green SJ, Voigt RM, Forsyth CB, Keshavarzian A. The Gastrointestinal Microbiome: Alcohol Effects on the Composition of Intestinal Microbiota. Alcohol Res. 2015;37(2):223-36. PMID: 26695747; PMCID: PMC4590619. [cited 2021 Feb 2]
62. de Sousa RT, Zanetti MV, Brunoni AR, Machado-Vieira R. Challenging Treatment-Resistant Major Depressive Disorder: A Roadmap for Improved Therapeutics. Curr Neuropharmacol. 2015;13(5):616-35. doi: 10.2174/1570159×13666150630173522. PMID: 26467411; PMCID: PMC4761633. [cited 2021 Feb 2]
63. Keks N, Schwartz D, Hope J. Stopping and switching antipsychotic drugs. Aust Prescr. 2019;42(5):152-157. doi:10.18773/austprescr.2019.052 [cited 2021 Feb 2]

 Open Dialogue and CBT are two forms of effective psychotherapy 11-15
Open Dialogue and CBT are two forms of effective psychotherapy 11-15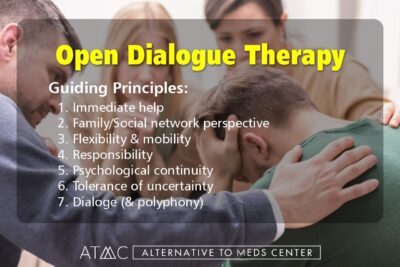 There is a residential approach to the treatment of psychiatric symptoms such as schizophrenia called Open Dialogue. This mode of treatment was originally introduced in Finland and has become popular in other parts of the world as well. Benefits have been reported as less need for medication, fewer symptoms of psychosis, less frequent hospitalizations, and increased numbers of persons being able to re-enter the workforce.11
There is a residential approach to the treatment of psychiatric symptoms such as schizophrenia called Open Dialogue. This mode of treatment was originally introduced in Finland and has become popular in other parts of the world as well. Benefits have been reported as less need for medication, fewer symptoms of psychosis, less frequent hospitalizations, and increased numbers of persons being able to re-enter the workforce.11 Alternative to Meds Center uses organic, clean food to design a diet that is not only crafted to be delicious but conducive to the reduction of sensitivities, balancing blood sugar, restoring needed nutrients that support a healthy microbiome, and
Alternative to Meds Center uses organic, clean food to design a diet that is not only crafted to be delicious but conducive to the reduction of sensitivities, balancing blood sugar, restoring needed nutrients that support a healthy microbiome, and 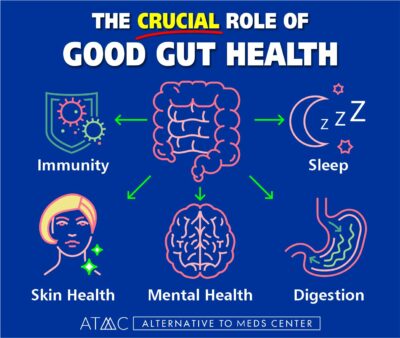 A link has been discovered between the gut and the CNS that is of significance when a person wants to stabilize the neurochemistry. This link is termed the “gut-brain axis.”
A link has been discovered between the gut and the CNS that is of significance when a person wants to stabilize the neurochemistry. This link is termed the “gut-brain axis.” Vitamins are essential for both physical and mental health. Each vitamin has numerous effects on the beautifully complex physical body. For example, vitamin E protects cell walls. Niacin is important for energy metabolism and the digestive tract (gut).10 Deficiencies can wreak havoc.
Vitamins are essential for both physical and mental health. Each vitamin has numerous effects on the beautifully complex physical body. For example, vitamin E protects cell walls. Niacin is important for energy metabolism and the digestive tract (gut).10 Deficiencies can wreak havoc. Even the drug companies admit that drugs stop working due to building tolerance to them over time.3,5
Even the drug companies admit that drugs stop working due to building tolerance to them over time.3,5 We have helped many of our clients who had an initial psychotic or bipolar episode to gradually reduce or eliminate their antipsychotic medications successfully. We use a thorough, gentle, and comprehensive approach that allows enough time to adjust, and heal which is greatly helped by utilizing natural alternatives to Seroquel and other harsh drugs.
We have helped many of our clients who had an initial psychotic or bipolar episode to gradually reduce or eliminate their antipsychotic medications successfully. We use a thorough, gentle, and comprehensive approach that allows enough time to adjust, and heal which is greatly helped by utilizing natural alternatives to Seroquel and other harsh drugs.