1. Kråkvik B, Gråwe RW, Hagen R, Stiles TC. Cognitive behaviour therapy for psychotic symptoms: a randomized controlled effectiveness trial. Behav Cogn Psychother. 2013;41(5):511-524. doi:10.1017/S1352465813000258 [cited 2022 July 29]
2. Amminger GP, Schäfer MR, Papageorgiou K, Klier CM, Cotton SM, Harrigan SM, Mackinnon A, McGorry PD, Berger GE. Long-chain omega-3 fatty acids for indicated prevention of psychotic disorders: a randomized, placebo-controlled trial. Arch Gen Psychiatry. 2010 Feb;67(2):146-54. doi: 10.1001/archgenpsychiatry.2009.192. PMID: 20124114. [cited 2022 July 29]
3. APA Div 12, Society of Clinical Psychology, “What is Exposure Therapy?” Clinical Practice Guidelines, [Internet] 2017 Jul [cited 2022 July 29]
4. “Antipsychotics- What if I don’t want to take antipsychotics?” Information letter published online by MIND For Better Health [cited 2022 July 29]
5. Sathyanarayana Rao TS, Asha MR, Ramesh BN, Jagannatha Rao, “Understanding nutrition, depression, and mental illness.” Indian Journal of Psychiatry [Internet] 2008 Apr-Jun [cited 2022 July 29]
6. Huang Q, Liu H, Suzuki K, Ma S, Liu C. Linking What We Eat to Our Mood: A Review of Diet, Dietary Antioxidants, and Depression. Antioxidants (Basel). 2019;8(9):376. Published 2019 Sep 5. doi:10.3390/antiox8090376 [cited 2022 July 29]
7. Psychosis with Methylphenidate or Amphetamine in Patients with ADHD Lauren V. Moran, M.D., Dost Ongur, M.D., Ph.D., John Hsu, M.D., M.S.C.E., Victor M. Castro, M.S., Roy H. Perlis, M.D., and Sebastian Schneeweiss, M.D., Sc.D. March 21, 2019 N Engl J Med 2019; 380:1128-1138 DOI: 10.1056/NEJMoa1813751.[cited 2022 July 29]
8. Glasner-Edwards S, Mooney LJ. Methamphetamine psychosis: epidemiology and management. CNS Drugs. 2014 Dec;28(12):1115-26. doi: 10.1007/s40263-014-0209-8. PMID: 25373627; PMCID: PMC5027896. [cited 2022 July 29]
9. Wang P, Si T. Use of antipsychotics in the treatment of depressive disorders. Shanghai Arch Psychiatry. 2013;25(3):134-140. doi:10.3969/j.issn.1002-0829.2013.03.002.[cited 2022 July 29]
10. Williams HJ, Owen MJ, O’Donovan MC. Is COMT a susceptibility gene for schizophrenia?. Schizophr Bull. 2007;33(3):635-641. doi:10.1093/schbul/sbm019. [cited [cited 2022 July 29]
11. Ira E, Zanoni M, Ruggeri M, Dazzan P, Tosato S. COMT, neuropsychological function and brain structure in schizophrenia: a systematic review and neurobiological interpretation. J Psychiatry Neurosci. 2013;38(6):366-380. doi:10.1503/jpn.120178. [cited 2022 July 29]
12. Acute Hypoglycemia Presenting as Acute Psychosis Tanveer Padder MD, Aparna Udyawar MD, Nouman Azhar MD, Kamil Jaghab MD From the Department of Psychiatry, Nassau University Medical Center, 2201 Hempstead Turnpike, East Meadow NY 11554 USA.First Published December 2005. [cited 2022 July 29]
13. Brady WJ Jr, Duncan CW. Hypoglycemia masquerading as acute psychosis and acute cocaine intoxication. Am J Emerg Med. 1999 May;17(3):318-9. doi: 10.1016/s0735-6757(99)90140-7. PMID: 10337905.[cited 2022 July 29]
14. Cannabis-Induced Psychosis: A Review Psychiatric Times, Vol 34 No 7, Volume 34, Issue 7July 14, 2017 Ruby S. Grewal, MD , Tony P. George, MD, FRCPC. [cited 2022 July 29]
15. Arendt M, Rosenberg R, Foldager L, Perto G, Munk-Jørgensen P. Cannabis-induced psychosis and subsequent schizophrenia-spectrum disorders: follow-up study of 535 incident cases. Br J Psychiatry. 2005 Dec;187:510-5. doi: 10.1192/bjp.187.6.510. PMID: 16319402. [cited 2022 July 29]
16. Rottanburg D, Robins AH, Ben-Arie O, Teggin A, Elk R. Cannabis-associated psychosis with hypomanic features Lancet. 1982 Dec 18;2(8312):1364-6. doi: 10.1016/s0140-6736(82)91270-3. PMID: 6129463. [cited 2022 July 29]
17. Understanding nutrition, depression and mental illnesses Indian J Psychiatry. 2008 Apr-Jun; 50(2): 77–82. T. S. Sathyanarayana Rao, M. R. Asha, B. N. Ramesh, and K. S. Jagannatha Rao [cited 2022 July 29]
18. Environmental Exposures and Depression: Biological Mechanisms and Epidemiological Evidence Annual Review of Public Health Vol. 40:239-259 (Volume publication date April 2019) First published as a Review in Advance 2019 Jan 11 [cited 2022 July 29]
19. Health Quality Ontario . Cognitive Behavioural Therapy for Psychosis: A Health Technology Assessment. Ont Health Technol Assess Ser. 2018;18(5):1-141. Published 2018 Oct 24.[cited 2022 July 29]
20. Seikkula J, Olson ME. The open dialogue approach to acute psychosis: its poetics and micropolitics. Fam Process. 2003 Fall;42(3):403-18. doi: 10.1111/j.1545-5300.2003.00403.x. PMID: 14606203. [cited 2022 July 29]
21. van den Berg DP, de Bont PA, van der Vleugel BM, de Roos C, de Jongh A, Van Minnen A, van der Gaag M. Prolonged exposure vs eye movement desensitization and reprocessing vs waiting list for posttraumatic stress disorder in patients with a psychotic disorder: a randomized clinical trial. JAMA Psychiatry. 2015 Mar;72(3):259-67. doi: 10.1001/jamapsychiatry.2014.2637. PMID: 25607833. [cited 2022 July 29]
22. Mental Health Medications National Institute of Mental Health Last Revised: October 2016[cited 2022 July 29]
23. Better Off Without Antipsychotic Drugs? June 18, 2014 E. Fuller Torrey, MD Psychiatric Times, Vol 31 No 6, Volume 31, Issue 6 [cited 2022 July 29]
24. Long-term Prognosis and Followup in Schizophrenia Joseph H. Stephens Author Notes Schizophrenia Bulletin, Volume 4, Issue 1, 1978, Pages 25–47, Published: 01 January 1978. [cited 2022 July 29]
25. Psychosocial Intervention With or Without Antipsychotic Medication for First-Episode Psychosis: A Randomized Noninferiority Clinical Trial
Shona M Francey, Brian O’Donoghue, Barnaby Nelson, Jessica Graham, Lara Baldwin, Hok Pan Yuen, Melissa J Kerr, Aswin Ratheesh, Kelly Allott, Mario Alvarez-Jimenez Schizophrenia Bulletin Open, Volume 1, Issue 1, January 2020, Published: 20 March 2020. [cited 2022 July 29]
26. Hoffer A, Osmond H. TREATMENT OF SCHIZOPHRENIA WITH NICOTINIC ACID. A TEN YEAR FOLLOW-UP. Acta Psychiatr Scand. 1964;40(2):171-89. doi: 10.1111/j.1600-0447.1964.tb05744.x. PMID: 14235254. [cited 2022 July 29]
27. Department of Psychiatry UC San Diego School of Medicine Preparing Open Dialogue Approach for Implementation in the U.S. [cited 2022 July 29]
28. Antipsychotics: Taking the Long View Ethics & Psychology, by Former NIMH Director Thomas Insel on August 28, 2013 [cited 2022 July 29]
29. Lakhan SE, Vieira KF. Nutritional therapies for mental disorders. Nutr J. 2008;7:2. Published 2008 Jan 21. doi:10.1186/1475-2891-7-2 [cited 2022 July 29]
30. Kraal A, Z, Arvanitis N, R, Jaeger A, P, Ellingrod V, L: Could Dietary Glutamate Play a Role in Psychiatric Distress? Neuropsychobiology 2020;79:13-19. doi: 10.1159/000496294 [cited 2022 July 29]
31. Plitman E, Nakajima S, de la Fuente-Sandoval C, et al. Glutamate-mediated excitotoxicity in schizophrenia: a review. Eur Neuropsychopharmacol. 2014;24(10):1591-1605. doi:10.1016/j.euroneuro.2014.07.015. [cited 2022 July 29]
32. van der Heijden, F., Fekkes, D., Tuinier, S. et al. Amino acids in schizophrenia: evidence for lower tryptophan availability during treatment with atypical antipsychotics?. J Neural Transm 112, 577–585 (2005). [cited 2022 July 29]
33. Christensen O, Christensen E, Fat consumption and schizophrenia Acta Psychiatrica Scandinavica [published: November 1988] [cited 2022 July 29]
34. Malcolm Peet, Eicosapentaenoic acid in the treatment of schizophrenia and depression: rationale and preliminary double-blind clinical trial results, Prostaglandins, Leukotrienes and Essential Fatty Acids, Science Direct, Volume 69, Issue 6, 2003, Pages 477-485. [cited 2022 July 29]
35. Leonardo Tondo, Nereide Rudas, The course of a seasonal bipolar disorder influenced by caffeine, Journal of Affective Disorders, Volume 22, Issue 4, 1991, Pages 249-251. [cited 2022 July 29]
36. Environmental Exposures and Depression: Biological Mechanisms and Epidemiological Evidence Annual Review of Public Health Vol. 40:239-259 (Volume publication date April 2019) First published as a Review in Advance on 2019 Jan 11 [cited 2022 July 29]
37. Mittal VA, Vargas T, Osborne KJ, et al. Exercise Treatments for Psychosis: A Review. Curr Treat Options Psychiatry. 2017;4(2):152-166. doi:10.1007/s40501-017-0112-2. [cited 2022 July 29]
38. Collaborative on Mental Health and the Environment Mental Health and Environmental Exposures from the Learning and Developmental Disabilities Initiative, November 2008. [cited 2022 July 29]
39. Does treatment of schizophrenia with antipsychotic medications eliminate or reduce psychosis? A 20-year multi-follow-up study Published online by Cambridge University Press: 24 March 2014 M. Harrow, T. H. Jobe and R. N. Faull. [cited 2022 July 29]
40. Ho BC, Andreasen NC, Ziebell S, Pierson R, Magnotta V. Long-term antipsychotic treatment and brain volumes: a longitudinal study of first-episode schizophrenia. Arch Gen Psychiatry. 2011 Feb;68(2):128-37. doi: 10.1001/archgenpsychiatry.2010.199. PMID: 21300943; PMCID: PMC3476840. [cited 2022 July 29]
41. Antipsychotic Drugs, Their Harmful Effects, and the Limits of Tort Reform Huffpost By Peter R. Breggin M.D. 11/01/2009 02:18pm EST | Updated November 17, 2011. [cited 2022 July 29]
42. Tost H, Alam T, Meyer-Lindenberg A. Dopamine and psychosis: theory, pathomechanisms and intermediate phenotypes. Neurosci Biobehav Rev. 2010;34(5):689-700. doi:10.1016/j.neubiorev.2009.06.005. [cited 2022 July 29]
43. Know your brain: Reward system Neuroscientifically Challenged January 16, 2015. [cited 2022 July 29]
44. A H Ashok, T R Marques, S Jauhar, M M Nour, M Goodwin, A H Young, and O D Howes. The dopamine hypothesis of bipolar affective disorder: the state of the art and implications for treatment Mol Psychiatry. 2017 May; 22(5): 666–679. Published online 2017 Mar 14. doi: 10.1038/mp.2017.16 [cited 2022 July 29]
45. Bové J, Prou D, Perier C, Przedborski S. Toxin-induced models of Parkinson’s disease. NeuroRx. 2005;2(3):484-494. doi:10.1602/neurorx.2.3.484 [cited 2022 July 29]
46. Farina M, Aschner M, da Rocha JBT. The catecholaminergic neurotransmitter system in methylmercury-induced neurotoxicity. Adv Neurotoxicol. 2017;1:47-81. doi:10.1016/bs.ant.2017.07.002 [cited 2022 July 29]
47. Liu C, Jiao C, Wang K, Yuan N. DNA Methylation and Psychiatric Disorders. Prog Mol Biol Transl Sci. 2018;157:175-232. doi: 10.1016/bs.pmbts.2018.01.006. Epub 2018 Apr 11. PMID: 29933950. [cited 2022 July 29]
48. Orthomolecular Treatment of Orthomolecular Schizophrenia Association of Great Britain; London, England, September 28-30, 1971. A. Hoffer, M.D., Ph.D., F.A.P.A. [cited 2022 July 29]
49. Kim EJ, Lim SY, Lee HJ, Lee JY, Choi S, Kim SY, Kim JM, Shin IS, Yoon JS, Yang SJ, Kim SW. Low dietary intake of n-3 fatty acids, niacin, folate, and vitamin C in Korean patients with schizophrenia and the development of dietary guidelines for schizophrenia. Nutr Res. 2017 Sep;45:10-18. doi: 10.1016/j.nutres.2017.07.001. Epub 2017 Jul 19. PMID: 29037327. [cited 2022 July 29]

 Clean diet: omit sugars, refined carbs, and processed foods. Choose organic if possible 6
Clean diet: omit sugars, refined carbs, and processed foods. Choose organic if possible 6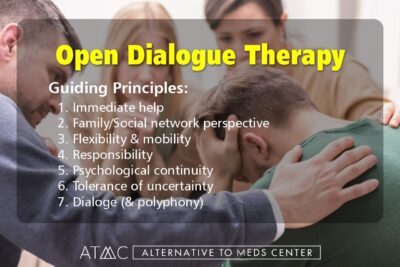 Prescribing these medications to children puts them at risk, as one of the common side effects that can occur especially in the first month or two of treatment with these drugs is suicidal thoughts or behavior.
Prescribing these medications to children puts them at risk, as one of the common side effects that can occur especially in the first month or two of treatment with these drugs is suicidal thoughts or behavior. Antipsychotic alternatives in a specialized treatment plan will usually contain more than just one treatment. Treatment plans can combine several or many different therapies. Through talk therapy of various kinds, patients can honestly express themselves, face their fears, better understand their illness, and begin to identify triggers and learn how to prevent and control them. For instance, cognitive-behavioral therapy helps patients to undo negative or unhealthy thought and behavior patterns, as well as rationalize fears and anxieties, balance mood swings, and continuously and gradually work towards a more complete internal peace.
Antipsychotic alternatives in a specialized treatment plan will usually contain more than just one treatment. Treatment plans can combine several or many different therapies. Through talk therapy of various kinds, patients can honestly express themselves, face their fears, better understand their illness, and begin to identify triggers and learn how to prevent and control them. For instance, cognitive-behavioral therapy helps patients to undo negative or unhealthy thought and behavior patterns, as well as rationalize fears and anxieties, balance mood swings, and continuously and gradually work towards a more complete internal peace. In a 1951 double-blind pilot study with 30 schizophrenics, Dr. Abram Hoffer MD, a Canadian psychiatrist, found that out of the 10 patients receiving nicotinic acid (a niacin type) seven of them had remained well during the one-year study. Another 10 patients were taking nicotinamide (another type of niacin) and “seven or eight had remained well,” while out of ten placebo patients, only three had remained well. That means approximately “75% of the patients receiving vitamins [niacin] had remained well, whereas only one-third of the patients receiving placebo had remained well.” 48 Dr. Hoffer then did a ten-year-long double-blind study using niacin and high-dose vitamin C. Hoffer claimed a 75% cure rate meaning that subjects endured a 5-year-long period of not having hospital readmission. Hoffer’s work laid the paving stones for what would later be termed orthomolecular medicine.26 Alternative to Meds Center uses these
In a 1951 double-blind pilot study with 30 schizophrenics, Dr. Abram Hoffer MD, a Canadian psychiatrist, found that out of the 10 patients receiving nicotinic acid (a niacin type) seven of them had remained well during the one-year study. Another 10 patients were taking nicotinamide (another type of niacin) and “seven or eight had remained well,” while out of ten placebo patients, only three had remained well. That means approximately “75% of the patients receiving vitamins [niacin] had remained well, whereas only one-third of the patients receiving placebo had remained well.” 48 Dr. Hoffer then did a ten-year-long double-blind study using niacin and high-dose vitamin C. Hoffer claimed a 75% cure rate meaning that subjects endured a 5-year-long period of not having hospital readmission. Hoffer’s work laid the paving stones for what would later be termed orthomolecular medicine.26 Alternative to Meds Center uses these  The answers to why an individual has experienced psychosis are specific for each person. However, our experience has revealed some common denominators of interest. For instance, one neurochemical believed to be significant in psychosis is the presence of excessive dopamine or disinhibited dopamine receptors.42 Dopamine is an excitatory neurochemical that is involved with the perception of reward.43 An excess of dopamine may cause internal preoccupations and external stimuli to overstimulate the person, which can result in mania.44 It is known that certain catecholaminergic neurotoxins can affect dopamine in parkinsonian patients.45 Similar toxins or even distinct toxins may also have an effect on dopamine levels as it relates to mania. Methyl mercury for instance has been attributed to dopamine excitotoxicity and dopamine excess.46 For this reason, we feel that exposure to certain neurotoxins is likely to contribute in whole or in part to mania or psychosis. Also, a genetic problem may present difficulties in clearing toxins from the body. For example, an insufficient methylator may be unable to get rid of toxic heavy metals. As a defense mechanism, these toxins may be stored in the brain, nerve, and other tissues.47
The answers to why an individual has experienced psychosis are specific for each person. However, our experience has revealed some common denominators of interest. For instance, one neurochemical believed to be significant in psychosis is the presence of excessive dopamine or disinhibited dopamine receptors.42 Dopamine is an excitatory neurochemical that is involved with the perception of reward.43 An excess of dopamine may cause internal preoccupations and external stimuli to overstimulate the person, which can result in mania.44 It is known that certain catecholaminergic neurotoxins can affect dopamine in parkinsonian patients.45 Similar toxins or even distinct toxins may also have an effect on dopamine levels as it relates to mania. Methyl mercury for instance has been attributed to dopamine excitotoxicity and dopamine excess.46 For this reason, we feel that exposure to certain neurotoxins is likely to contribute in whole or in part to mania or psychosis. Also, a genetic problem may present difficulties in clearing toxins from the body. For example, an insufficient methylator may be unable to get rid of toxic heavy metals. As a defense mechanism, these toxins may be stored in the brain, nerve, and other tissues.47 At Alternative to Meds Center, our
At Alternative to Meds Center, our