1. Alladi, Charanraj Goud et al. “Risperidone-Induced Adverse Drug Reactions and Role of DRD2 (-141 C Ins/Del) and 5HTR2C (-759 C>T) Genetic Polymorphisms in Patients with Schizophrenia.” Journal of pharmacology & pharmacotherapeutics vol. 8,1 (2017): 28-32. doi:10.4103/jpp.JPP_197_16 [cited 2022 June 24]
2. Matthews Maju, Gratz S, Adetunji B, George V, Matthews Manu, Biju B “Antipsychotic-Induced Movement Disorders – Evaluation and Treatment.” Psychiatry MMC Journal [Internet] 2005 Mar [cited 2022 June 22]
3. Lee PE, Sykora K, Gill SS, Mamdani M, Marras C, Anderson G, Shulman KI, Stukel T, Normand SL, Rochon PA. Antipsychotic medications and drug-induced movement disorders other than parkinsonism: a population-based cohort study in older adults. J Am Geriatr Soc. 2005 Aug;53(8):1374-9. doi: 10.1111/j.1532-5415.2005.53418.x. PMID: 16078964. [cited 2022 June 24]
4. Stevović LI, Repišti S, Radojičić T, Sartorius N, Tomori S, Džubur Kulenović A, Popova A, Kuzman MR, Vlachos II, Statovci S, Bandati A, Novotni A, Bajraktarov S, Panfil AL, Maric NP, Delić M, Jovanović N. Non-pharmacological treatments for schizophrenia in Southeast Europe: An expert survey. Int J Soc Psychiatry. 2021 Aug 14:207640211023072. doi: 10.1177/00207640211023072. Epub ahead of print. PMID: 34392727. [cited 2022 June 24]
5. Fogel DB. Factors associated with clinical trials that fail and opportunities for improving the likelihood of success: A review. Contemp Clin Trials Commun. 2018;11:156-164. Published 2018 Aug 7. doi:10.1016/j.conctc.2018.08.001 [cited 2022 June 24]
6. Aucoin M, LaChance L, Clouthier SN, Cooley K. Dietary modification in the treatment of schizophrenia spectrum disorders: A systematic review. World J Psychiatry. 2020 Aug 19;10(8):187-201. doi: 10.5498/wjp.v10.i8.187. PMID: 32874956; PMCID: PMC7439299. [cited 2022 June 22]
7. McCarthy M, Companies to pay $39.5m in OxyContin and Risperdal cases. BMJ 2015;351:h7018 [cited 2022 June 24]
8. Aucoin M, LaChance L, Cooley K, Kidd S. Diet and Psychosis: A Scoping Review. Neuropsychobiology. 2020;79(1):20-42. doi: 10.1159/000493399. Epub 2018 Oct 25. PMID: 30359969.[cited 2022 June 22]
9. Dickerson F, Stallings C, Origoni A, Vaughan C, Khushalani S, Yolken R. Markers of gluten sensitivity in acute mania: a longitudinal study. Psychiatry Res. 2012 Mar 30;196(1):68-71. doi: 10.1016/j.psychres.2011.11.007. Epub 2012 Mar 3. PMID: 22386570. [cited 2022 June 22]
10. Samaroo D, Dickerson F, Kasarda DD, et al. Novel immune response to gluten in individuals with schizophrenia.Schizophr Res. 2010;118(1-3):248-255. doi:10.1016/j.schres.2009.08.009 [cited 2022 June 22]
11. Arinola G, Idonije B, Akinlade K, Ihenyen O. Essential trace metals and heavy metals in newly diagnosed schizophrenic patients and those on anti-psychotic medication. J Res Med Sci. 2010;15(5):245-249.[cited 2022 June 22]
12. MAGHAZAJI H I, Psychiatric aspects of methylmercury poisoning Journal of Neurology, Neurosurgery, and Psychiatry, 1974, 37, 954-958 From the Department of Medicine, Medical College, Baghdad University [cited 2022 June 24]
13. Aschner, M., Walker, S. The neuropathogenesis of mercury toxicity. Mol Psychiatry 7, S40–S41 (2002). [cited 2022 June 24]
14. Xuebing Huang, Samuel Law, Dan Li, Xin Yu, Bing Li, Mercury Poisoning: A Case of a Complex Neuropsychiatric Illness The American Journal of Psychiatry [cited 2022 June 24]
15. FDA label Risperdal (risperidone) approval 1993 Revised June 2009 [cited 2022 June 22]
16. David D, Cristea I, Hofmann SG. Why Cognitive Behavioral Therapy Is the Current Gold Standard of Psychotherapy. Front Psychiatry. 2018;9:4. Published 2018 Jan 29. doi:10.3389/fpsyt.2018.00004 [cited 2022 June 22]
17. Kraeuter AK, Phillips R, Sarnyai Z. The Gut Microbiome in Psychosis From Mice to Men: A Systematic Review of Preclinical and Clinical Studies. Front Psychiatry. 2020;11:799. Published 2020 Aug 11. doi:10.3389/fpsyt.2020.00799 [cited 2022 June 22]
18. Nguyen T T, Hathaway H, Kosciolek T, Knight R, Jeste D V, Gut microbiome in serious mental illnesses: A systematic review and critical evaluation, Schizophrenia Research, 2019, Aug 26, ISSN 0920-9964 [cited 2022 June 24]
19. Emily G. Severance, Robert H. Yolken, William W. Eaton, Autoimmune diseases, gastrointestinal disorders and the microbiome in schizophrenia: more than a gut feeling, Schizophrenia Research, Volume 176, Issue 1, 2016, Pages 23-35, ISSN 0920-9964, [cited 2022 June 22]
20. Levinta A, Mukovozov I, Tsoutsoulas C. Use of a Gluten-Free Diet in Schizophrenia: A Systematic Review. Adv Nutr. 2018;9(6):824-832. doi:10.1093/advances/nmy056 [cited 2022 June 24]
21. Khalil RM, Khedr NF. Curcumin Protects against Monosodium Glutamate Neurotoxicity and Decreasing NMDA2B and mGluR5 Expression in Rat Hippocampus. Neurosignals. 2016;24(1):81-87. doi: 10.1159/000442614. Epub 2016 Aug 17. PMID: 27529496. [cited 2022 June 22]
22. Padder T, et al, Acute Hypoglycemia Presenting as Acute Psychosis Published December 2005 Priory Lodge Education [cited 2022 June 22]
23. Brady WJ Jr, Duncan CW. Hypoglycemia masquerading as acute psychosis and acute cocaine intoxication. Am J Emerg Med. 1999 May;17(3):318-9. doi: 10.1016/s0735-6757(99)90140-7. PMID: 10337905. [cited 2022 June 22]
24. Leonardo Tondo, Nereide Rudas, The course of a seasonal bipolar disorder influenced by caffeine, Journal of Affective Disorders, Volume 22, Issue 4, 1991, Pages 249-251. [cited 2022 June 22]
25. Understanding nutrition, depression and mental illnesses Indian J Psychiatry. 2008 Apr-Jun; 50(2): 77–82. T. S. Sathyanarayana Rao, M. R. Asha, B. N. Ramesh, and K. S. Jagannatha Rao [cited 2022 June 22]
26. van der Heijden, F., Fekkes, D., Tuinier, S. et al. Amino acids in schizophrenia: evidence for lower tryptophan availability during treatment with atypical antipsychotics?. J Neural Transm 112, 577–585 (2005). [cited 2022 June 22]
27. Christensen O, Christensen E, Fat consumption and schizophrenia Acta Psychiatrica Scandinavica November 1988. [cited 2022 June 24]
28. McNamara R K, “Mitigation of Inflammation-Induced Mood Dysregulation by Long-Chain Omega-3 Fatty Acids.” Journal of American College of Nutrition [Internet] 2015;34 Suppl 1(0 1):48-55. DOI: 10.1080/07315724.2015.1080527 [cited 2022 June 22]
29. Malcolm Peet, Eicosapentaenoic acid in the treatment of schizophrenia and depression: rationale and preliminary double-blind clinical trial results, Prostaglandins, Leukotrienes and Essential Fatty Acids, Science Direct, Volume 69, Issue 6, 2003, Pages 477-485. [cited 2022 June 24]
30. Gurusamy J, Gandhi S, Damodharan D, Ganesan V, Palaniappan M. Exercise, diet and educational interventions for metabolic syndrome in persons with schizophrenia: A systematic review. Asian J Psychiatr. 2018 Aug;36:73-85. doi: 10.1016/j.ajp.2018.06.018. Epub 2018 Jun 30. PMID: 29990631. [cited 2022 June 22]
31. National Research Council (US) Committee on Diet and Health. Diet and Health: Implications for Reducing Chronic Disease Risk. Washington (DC): National Academies Press (US); 1989. 14, Trace Elements. [cited 2022 June 22]
32. Cain L, LOW-DOSE LITHIUM: AN EFFECTIVE TREATMENT FOR MOOD DISORDERS Naturopathic Doctor News and Review Published online 2020 Mar 2 [cited 2022 June 24]
33. H.E. Sartori, Lithium orotate in the treatment of alcoholism and related conditions, Alcohol, Volume 3, Issue 2, 1986, Pages 97-100, ISSN 0741-8329. [cited 2022 June 22]
34. Aucoin M, LaChance L, Clouthier SN, Cooley K. Dietary modification in the treatment of schizophrenia spectrum disorders: A systematic review. World J Psychiatry. 2020 Aug 19;10(8):187-201. doi: 10.5498/wjp.v10.i8.187. PMID: 32874956; PMCID: PMC7439299. [cited 2022 June 22]
35. Pacholko AG, Bekar LK. Lithium orotate: A superior option for lithium therapy? Brain Behav. 2021 Jul 1. doi: 10.1002/brb3.2262. Epub ahead of print. PMID: 34196467. [cited 2022 June 22]
36. Kling MA, Manowitz P, Pollack IW. Rat brain and serum lithium concentrations after acute injections of lithium carbonate and orotate. J Pharm Pharmacol. 1978 Jun;30(6):368-70. doi: 10.1111/j.2042-7158.1978.tb13258.x. PMID: 26768. [cited 2022 June 22]
37. Sher L. Suicide in men. J Clin Psychiatry. 2015 Mar;76(3):e371-2. doi: 10.4088/JCP.14com09554. PMID: 25830461. [cited 2022 June 24]
38. Schrauzer, G.N., Shrestha, K.P. Lithium in drinking water and the incidences of crimes, suicides, and arrests related to drug addictions. Biol Trace Elem Res 25, 105–113 (1990). [cited 2022 June 22]
39. Cipriani A, Hawton K, Stockton S, Geddes J R Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis BMJ 2013; 346 (Published 27 June 2013) [cited 2022 June 24]
40. Hoffer A, Osmond H. TREATMENT OF SCHIZOPHRENIA WITH NICOTINIC ACID. A TEN YEAR FOLLOW-UP. Acta Psychiatr Scand. 1964;40(2):171-89. doi: 10.1111/j.1600-0447.1964.tb05744.x. PMID: 14235254. [cited 2022 June 22]
41. Hoffer A, Orthomolecular Treatment of Schizophrenia [September 28-30, 1971] [cited 2022 June 22]
42. Environmental Exposures and Depression: Biological Mechanisms and Epidemiological Evidence Annual Review of Public Health Vol. 40:239-259 (Volume publication date April 2019) First published as a Review in Advance on 2019 Jan 11 [cited 2022 June 22]
43. Collaborative on Mental Health and the Environment Mental Health and Environmental Exposures from the Learning and Developmental Disabilities Initiative, November 2008. [cited 2022 June 22]
44. Mittal VA, Vargas T, Osborne KJ, et al. Exercise Treatments for Psychosis: A Review. Curr Treat Options Psychiatry. 2017;4(2):152-166. doi:10.1007/s40501-017-0112-2. [cited 2022 June 22]
45. Mead MN. Benefits of sunlight: a bright spot for human health [published correction appears in Environ Health Perspect. 2008 May;116(5):A197]. Environ Health Perspect. 2008;116(4):A160-A167. doi:10.1289/ehp.116-a160 [cited 2022 June 22]
46. Siebern AT, Suh S, Nowakowski S. Non-pharmacological treatment of insomnia. Neurotherapeutics. 2012;9(4):717-727. doi:10.1007/s13311-012-0142-9 [cited 2022 June 22]
47. Grewal R S, George T P, Cannabis-Induced Psychosis: A Review Psychiatric Times, Vol 34 No 7, Volume 34, Issue 7July 14, 2017 [cited 2022 June 24]
48. Arendt M, Rosenberg R, Foldager L, Perto G, Munk-Jørgensen P. Cannabis-induced psychosis and subsequent schizophrenia-spectrum disorders: follow-up study of 535 incident cases. Br J Psychiatry. 2005 Dec;187:510-5. doi: 10.1192/bjp.187.6.510. PMID: 16319402. [cited 2022 June 22]
49. Rottanburg D, Robins A H, Ben-Arie O, Teggin A, Elk R. Cannabis-associated psychosis with hypomanic features Lancet. 1982 Dec 18;2(8312):1364-6. doi: 10.1016/s0140-6736(82)91270-3. PMID: 6129463. [cited 2022 June 22]
50. Morrison AK. Cognitive behavior therapy for people with schizophrenia. Psychiatry (Edgmont). 2009;6(12):32-39. [cited 2022 June 22]
51. Freeman et al., “Open Dialogue: A Review of the Evidence.” published in Psychiatryonline 18 Oct 2018 [cited 2022 June 22]
52. Wilson G, Farrell D, Barron I, Hutchins J, Whybrow D, Kiernan MD. The Use of Eye-Movement Desensitization Reprocessing (EMDR) Therapy in Treating Post-traumatic Stress Disorder-A Systematic Narrative Review. Front Psychol. 2018;9:923. Published 2018 Jun 6. doi:10.3389/fpsyg.2018.00923 [cited 2022 June 22]
53. Frueh BC, Grubaugh AL, Cusack KJ, Kimble MO, Elhai JD, Knapp RG. Exposure-based cognitive-behavioral treatment of PTSD in adults with schizophrenia or schizoaffective disorder: a pilot study. J Anxiety Disord. 2009;23(5):665-675. doi:10.1016/j.janxdis.2009.02.005 [cited 2022 June 22]
54. Clapp M, Aurora N, Herrera L, Bhatia M, Wilen E, Wakefield S. Gut microbiota’s effect on mental health: The gut-brain axis. Clin Pract. 2017;7(4):987. Published 2017 Sep 15. doi:10.4081/cp.2017.987 [cited 2022 June 22]
55. Walker R, Lupien J R, The Safety Evaluation of Monosodium Glutamate, The Journal of Nutrition, Volume 130, Issue 4, April 2000, Pages 1049S–1052S [cited 2022 June 22]
56. Young S N. The effect of raising and lowering tryptophan levels on human mood and social behaviour. Philos Trans R Soc Lond B Biol Sci. 2013;368(1615):20110375. Published 2013 Feb 25. doi:10.1098/rstb.2011.0375 [cited 2022 June 22]
57. Lakhan S E, Vieira KF. Nutritional therapies for mental disorders. Nutr J. 2008;7:2. Published 2008 Jan 21. doi:10.1186/1475-2891-7-2 [cited 2022 June 22]
58. van der Heijden, F., Fekkes, D., Tuinier, S. et al. Amino acids in schizophrenia: evidence for lower tryptophan availability during treatment with atypical antipsychotics?. J Neural Transm 112, 577–585 (2005). [cited 2022 June 22]
59. Zemlan FP, Hirschowitz J, Sautter FJ, Garver DL. Impact of lithium therapy on core psychotic symptoms of schizophrenia. Br J Psychiatry. 1984 Jan;144:64-9. doi: 10.1192/bjp.144.1.64. PMID: 6419805. [cited 2022 June 24]
60. Bonaz B, Bazin T, Pellissier S. The Vagus Nerve at the Interface of the Microbiota-Gut-Brain Axis. Front Neurosci. 2018 Feb 7;12:49. doi: 10.3389/fnins.2018.00049. PMID: 29467611; PMCID: PMC5808284. [cited 2022 June 22]
61. Deiana S. Medical use of cannabis. Cannabidiol: a new light for schizophrenia? Drug Test Anal. 2013 Jan;5(1):46-51. doi: 10.1002/dta.1425. Epub 2012 Oct 25. PMID: 23109356. [cited 2022 June 22]
62. Batalla-Martín D, Belzunegui-Eraso A, Miralles Garijo E, Martínez Martín E, Romaní Garcia R, Heras JSM, Lopez-Ruiz M, Martorell-Poveda MA. Insomnia in Schizophrenia Patients: Prevalence and Quality of Life. Int J Environ Res Public Health. 2020 Feb 19;17(4):1350. doi: 10.3390/ijerph17041350. PMID: 32093111; PMCID: PMC7068578. [cited 2022 June 22]
63. Shechter A, Kim EW, St-Onge MP, Westwood AJ. Blocking nocturnal blue light for insomnia: A randomized controlled trial. J Psychiatr Res. 2018;96:196-202. doi:10.1016/j.jpsychires.2017.10.015 [cited 2022 June 22]
64. Mason LH, Mathews MJ, Han DY. Neuropsychiatric symptom assessments in toxic exposure. Psychiatr Clin North Am. 2013 Jun;36(2):201-8. doi: 10.1016/j.psc.2013.02.001. Epub 2013 Apr 15. PMID: 23688687. [cited 2022 June 22]
65. Tewksbury A, Olander A. Management of antipsychotic-induced hyperprolactinemia. Ment Health Clin. 2016;6(4):185-190. Published 2016 Jun 29. doi:10.9740/mhc.2016.07.185 [cited 2022 June 24]

 CBT and other genres of psychological therapy. 16
CBT and other genres of psychological therapy. 16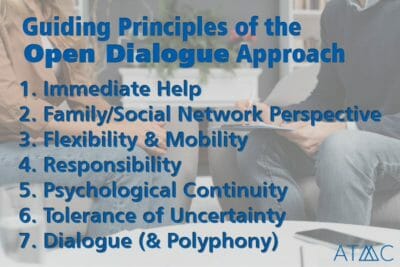 Morrison’s 2009 study on CBT in the treatment of schizophrenia found that the core symptoms of schizophrenia are often resistant to medication-based treatment, but can significantly improve with cognitive behavioral therapy. Benefits to family and other relationships, as well as improvements in the workplace, are noted, along with an expressed call for more research on this under-studied area of human health.50
Morrison’s 2009 study on CBT in the treatment of schizophrenia found that the core symptoms of schizophrenia are often resistant to medication-based treatment, but can significantly improve with cognitive behavioral therapy. Benefits to family and other relationships, as well as improvements in the workplace, are noted, along with an expressed call for more research on this under-studied area of human health.50 It is traditional for physicians to recommend beneficial modifications to diet, restricting sugars, and gluten, and making other changes.
It is traditional for physicians to recommend beneficial modifications to diet, restricting sugars, and gluten, and making other changes.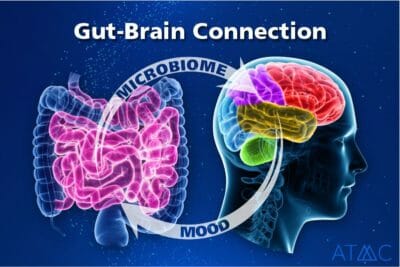 The microbiome is defined as all the microorganisms in the human body and their respective genetic material. Microbiota is the term used when focusing on a particular part of the body and the microorganisms found there. The condition of the microbiota of the gut is of particular interest in mental health. This connection is termed “the gut-brain axis.” The relationship between the gut and the brain develops from infancy and continues to develop throughout one’s life, involving hormones, bacteria, emotional responses, digestion, energy, organ function, and more. According to a review of clinical data, Nguyen et al suggest there are differences in the microbiota of the gut comparing schizophrenic patients and non-schizophrenic controls.18
The microbiome is defined as all the microorganisms in the human body and their respective genetic material. Microbiota is the term used when focusing on a particular part of the body and the microorganisms found there. The condition of the microbiota of the gut is of particular interest in mental health. This connection is termed “the gut-brain axis.” The relationship between the gut and the brain develops from infancy and continues to develop throughout one’s life, involving hormones, bacteria, emotional responses, digestion, energy, organ function, and more. According to a review of clinical data, Nguyen et al suggest there are differences in the microbiota of the gut comparing schizophrenic patients and non-schizophrenic controls.18 A host of
A host of 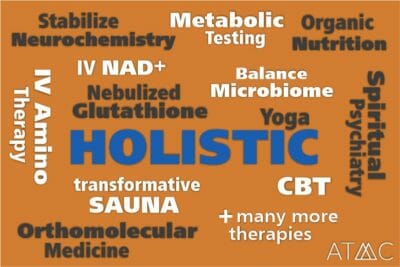 Our program includes medical professionals to aid individuals in reducing dependence upon Risperdal. This is done by utilizing carefully planned
Our program includes medical professionals to aid individuals in reducing dependence upon Risperdal. This is done by utilizing carefully planned