Last Updated on September 20, 2022 by
Alternative to Meds Editorial Team
Medically Reviewed by Dr Michael Loes MD
Table of Contents:
Don’t suffer needlessly if you are a veteran with PTSD who abuses drugs or alcohol. Help is available. Traumatic events, stress relief, and societal norms are contributing factors to the prevalence of substance abuse problems among military veterans.
According to the U.S. Department of Veterans Affairs, more than 20% of veterans with post-traumatic stress disorder (PTSD) also have substance abuse disorder (SUD). And nearly one-third of veterans seeking treatment for SUD also have PTSD.
Not everyone who is involved in a highly stressful event develops PTSD. In addition to exposure to trauma, the Mayo Clinic suggests that the disorder is caused by a complex mix of those experiences with inherited mental health risks. Temperament and how your brain regulates your body’s chemical response to stress also contribute.
Substance Abuse Treatment and Resources
Treatment centers, behavioral therapy, and other drug abuse treatment options are available for veterans of the armed forces suffering from PTSD and substance use problems, and for their families. Inpatient and outpatient care at treatment facilities are available.
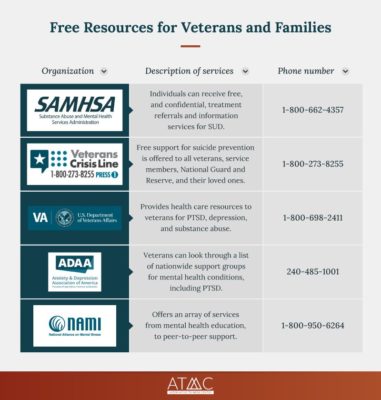
Resources for mental health treatment and support include:
Alternative to Meds Center, which offers drug-free treatment to help get veterans on the right track. The ATMC uses lab testing to determine physiological reasons for why guests may abuse alcohol. Therefore, the ATMC can tailor each program for each guest’s physiological needs. Call (888) 906-1547.
- The Substance Abuse and Mental Health Services Administration. SAMHSA is the national assistance hotline where people can receive free, and confidential treatment referrals, including information services for SUD. SAMHSA is free. For uninsured guests, SAMHSA refers guests to that individual guest’s state office, which is the office responsible for state-funded treatment programs.
- The Veterans Crisis Line is a resource that provides free support to all veterans, service members, National Guard and Reserve, and their loved ones, family members, and friends. The crisis line includes suicide prevention via text, chat, or phone: (800) 273-8255.
- The Department of Veterans Affairs offers VA health care resources for health problems including, but not limited to, PTSD, depression, and substance abuse.
- The Anxiety & Depression Association of America has a list of support groups nationwide for a variety of mental health conditions, including PTSD. Access the list at the ADAA’s website.
- The National Alliance on Mental Illness offers an array of services from mental health education, to peer-to-peer support.
- Addiction Group is a free helpline center that answers any questions you may have about substance abuse, addiction, and treatment options.
- Addiction Resource helps you locate alcohol and drug rehab options near you.
- Give an Hour is a national network that offers free mental health care services to active duty, National Guard and Reserve, veterans, and their loved ones.
- Lone Survivor Foundation is a virtual counseling program that helps veterans with PTSD symptoms. All expenses for this program are funded by the Lone Survivor Foundation’s sponsors.
- Sierra Tucson is a residential treatment center for drug and alcohol addiction, pain recovery, and behavioral health.
- USA Cares helps service members obtain treatment for post-traumatic stress disorder and/or traumatic brain injury (TBI).
- Coalition Peer Support Program is a veteran circle, connecting disabled veterans.
- PTSD Foundation of America is a free whole-person approach, offering evidence-based peer-to-peer mentoring, both on an individual basis and in group settings.
- PsychArmor Institute is an online education and support system for all Americans who work with, live with, or care for military service members, veterans, and their families.
- Disabled American Veterans is a nonprofit charity that provides a lifetime of support for veterans of all generations and their families.
- Purple Heart Foundation provides services, programs, and resources to help combat wounded and disabled veterans and their families with financial grants, claims assistance, PTSD resources, and employment counseling.
- American Addiction Centers provide resources to veterans who are struggling with PTSD symptoms.
- Military One Source provides access to contracted mental health counselors who will confidently speak with you about your concerns and offer targeted information that can help deal with difficult situations.
- PTSD United is a nonprofit organization dedicated to providing free resources for sufferers of PTSD, and their friends and family.
- Coaching into Care offers telephone coaching by licensed clinicians to educate, support, and empower family members and friends who are seeking care or services for a veteran.
- Home Base Veteran and Family Care offers a two-week Intensive clinical program that treats veterans with PTSD, traumatic brain injury (TBI), sexual trauma, depression, and anxiety.
- True REST Float Spa offers veterans one free hour of flotation therapy in a pod filled with a specialized solution of 1,000 pounds of Epsom salts and 180 gallons of water, allowing the body to float effortlessly. The practice has been proven to alleviate anxiety, depression, and chronic pain.
- Warrior Care Network partners with four academic medical centers to provide mental health services for post-Sept. 11 veterans. Participating veterans receive a year’s worth of care during a two- to three-week outpatient program.
- Operation Mend-Intensive Treatment Program serves active-duty service members, veterans, and their families impacted by service-related mild traumatic brain injury and PTSD.
- Real Warriors: The Real Warriors Campaign promotes a culture of support for psychological health by encouraging the military community to reach out for help, whether they’re coping with the daily stressors of military life or concerns like depression, anxiety, and PTSD.
- Motorcycle Relief Project invites veterans on guided motorcycle adventure trips to decompress and learn tools for managing stress.
- Outward Bound for Veterans offers wilderness expeditions that purposefully scaffold wartime experiences (carrying heavy packs, sore shoulders, rubbery legs, sleeping outdoors, strange noises, sweat, dirt, frustration, and anger) to help veterans return home after wartime service.
What is PTSD?
Post-traumatic stress disorder (PTSD) is a mental illness disorder that occurs in people who have experienced trauma at some time.
Some things that may cause PTSD can include:
- War/combat experience
- Sexual violence or rape
- Death threats
- Terrorist acts
- Serious accident or injury
PTSD is similar to, but not the same as acute stress disorder, or ASD. Like PTSD survivors, those with ASD may relive the trauma and have nightmares or flashbacks. They may feel numb or detach themselves from reality. Symptoms occur between three days and a month after the event.
Some symptoms of PTSD, by contrast, may remain longer than 50 years.
According to estimates, ASD affects:
- 13% to 21% of those in car accidents
- 20% to 50% of assault, rape, and mass-shooting survivors
Symptoms of PTSD
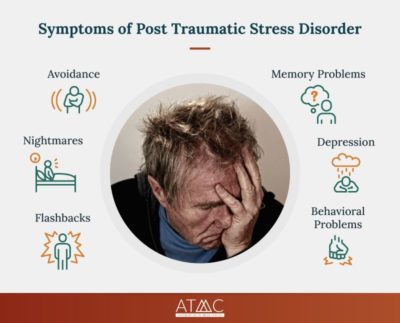
PTSD symptoms may increase with age, even occurring 50 years or more after the initial wartime event, for a number of reasons.
Retirement can increase symptoms by giving veterans more time to think about the past with fewer distractions. Plus, increased medical problems may make them feel less strong.
Some veterans who’ve used alcohol or other substances to cope in the past stop and become sober. If they are no longer able to become intoxicated because of health issues or for other reasons, they may find PTSD symptoms worsen.
What kind of symptoms might they experience?
They fall into three general categories: reliving the trauma; avoiding situations that can trigger memories of the event; and a highly irritable, anxious state.
-
- Flashbacks — There are several types of flashbacks. In visual flashbacks, you feel like you’re transported back to the moment of trauma and are going through it all over again. Somatic flashbacks trigger pain and discomfort in areas affected by the trauma. Emotional flashbacks cause intense, often irrational feelings.
- Nightmares — PTSD survivors are far more likely to experience nightmares. One study found that 52% of combat veterans with PTSD who served in Vietnam had nightmares fairly frequently. Meanwhile, only 3% of civilians reported comparable levels of nightmares. Some PTSD survivors may experience nightmares several times a week.
- Avoidance — PTSD survivors may attempt to cope by avoiding triggering situations or even avoiding the feelings themselves. But avoidance may make the symptoms even worse.
- Memory problems — Memory loss and trouble concentrating are common symptoms of PTSD. This is of concern because memory problems can impact a patient’s ability to respond to, and take part in, psychological treatment.
- Behavioral problems — Self-destructive behavior and irritability or aggression are among the behavioral problems associated with PTSD. They also are called arousal symptoms.
- Depression — About half of those affected by PTSD also suffer from major depressive disorder. This can create further challenges because those who have both disorders are more likely to drop out of treatment.
What is SUD?
Substance use disorder involves the misuse of potentially dangerous substances. People with SUD misuse alcohol, cocaine, opioids, or other addictive substances to the extent that it interferes with their well-being or daily activities. Work, school, or family life can suffer. It’s a diagnosable medical disorder, not a moral failing.
How does substance abuse affect veterans?
SUD often co-occurs with other disorders like PTSD, anxiety, and/or depression. According to one study, 51.9% of men and 27.9% of women who had lifetime PTSD also had SUD.
The National Vietnam Veterans Readjustment Study in the 1980s found that 74% of Vietnam veterans who had PTSD also had SUD. Alcohol abuse was a particular concern.Not only can drinking serve as an attempt to self-medicate against the effects of PTSD, but it also serves a social function within the military. During active duty, 1 in 3 service members is a binge drinker. And binge drinking is more common among those with high combat exposure.
More than 65% of veterans in addiction treatment reported that alcohol was their primary substance of abuse. Alcohol is readily available, both within the U.S. military and the general population. So its use among active-duty military service members affected by combat trauma, as well as by veterans with PTSD, is not surprising.
How Common are PTSD and SUD in Veterans?
The relationship between PTSD and SUD can be complex. In some cases, veterans develop SUD as an attempted coping mechanism to deal with PTSD. But it’s not always as simple as that. Some studies show that certain genes increase the risk of a person developing both SUD and PTSD, and some life events make both more likely.
There’s also an increased possibility that someone with SUD is more likely to be exposed to traumatic situations. Studies have shown that drug and alcohol use can affect the way the brain communicates, interfering with rational thought and making risky behavior more likely. That behavior, in turn, can lead to situations where trauma is more apt to occur.
For instance, a survey by the U.S. Department of Health and Human Services found that 40% of students who reported drinking said they’d blacked out at least once in the previous year.
This lack of sensory awareness could easily put them in a vulnerable position for trauma, if, to name one example, they were driving. Beyond that, drinking slows the reflexes, so reaction time can be delayed when a threat presents itself.
These are some of the reasons that alcohol is the third-leading preventable cause of death in the United States, behind tobacco and poor diet. About 68,000 men and 27,000 women die from alcohol-related causes each year.
About half of people diagnosed with PTSD develop SUD, and vice versa. About half of the people diagnosed with SUD will be exposed to traumatic situations or events that will cause them to develop PTSD.
Here are some other statistics about PTSD and SUD:
- More than 11% of the veterans who served in Afghanistan and Iraq have been diagnosed with SUD (10).
- About 22% of the veterans who served in Afghanistan and Iraq who had PTSD also had SUD (10).
- Approximately 82% to 93% of veterans diagnosed with substance use disorders were also diagnosed with mental health disorders, such as PTSD (5).
- One-third of veterans who experienced a traumatic brain injury met the criteria of PTSD (8).
- Approximately 300,000 veterans who returned from Iraq and Afghanistan are suffering from PTSD (8).
- Heavy episodic drinking and cigarette smoking are the two most prevalent types of substance-use issues among male and female veterans (5).
Substance Abuse in Veterans
As mentioned, active-duty service members are more likely to abuse alcohol. Heavy drinking often carries over among veterans because of the addictive nature of alcohol.
Alcohol addiction, like PTSD, is complex. For instance, studies have observed that the reward center in the brain responds differently in heavy drinkers than in light drinkers.
Heavy drinkers reported feeling more intoxicated after consuming the same amount of alcohol, suggesting they’re more easily affected by the release of endorphins in the brain. They get a feel-good “reward” for drinking that serves as an incentive to drink more.
This indicates genetic factors can predispose people to alcohol addiction. The continued reward provided by the release of endorphins can reinforce that predisposition.
What percentage of veterans abuse substances?
Nevertheless, exposure to trauma also plays a role in drinking behavior: Veterans who were exposed to more combat had a greater likelihood of engaging in heavy drinking and binge drinking.
Specifically, veterans with higher levels of combat exposure were more likely to:
- Heavily drink alcohol (26.8%)
- Binge drink alcohol (54.8%)
- Heavily drink alcohol (17%)
- Binge drink alcohol (45%)
- 3.5% of veterans reported marijuana use.
- 1.7% of veterans reported illicit drug use, not marijuana.
- Veterans are more likely than average civilians to smoke cigarettes (27% vs 21%).
- In 2013, approximately 62,000 veterans admitted themselves to substance-abuse treatment.
- Alcohol was the most common substance abuse among the group at 65.4%.
- In comparison, among nonveterans who sought treatment for substance abuse, only 37.4% were for alcohol use.
- Among veterans, the next highest substance abuse after alcohol was heroin at 10.7%.
- Among nonveterans, this percentage was twice as high, at about 20.9%.
Signs of Substance Abuse
Substance abuse and addiction, in general, can fall into more than one category.
Physical dependence is the body’s dependence on the drug and its chemical effects. Over time, the body builds up a tolerance to the drug and will need larger doses to have the same result. When you stop, withdrawal occurs. The same can be true for prescription drugs, such as painkillers.
Psychological dependence is an addiction based on how a drug makes you feel, often as a means of coping with chronic pain or negative situations or feelings. It isn’t the direct effect of the drugs on physical chemistry that causes the addiction. Rather, it’s the drugs’ psychological effect on the situation.
A third type of addiction is similar to psychological addiction, but not exactly the same. This type of addiction, behavioral addiction, is an addiction to a feeling caused by doing anything you find enjoyable. It doesn’t have to be a drug. It can involve things like gambling, pornography, shopping, video games, or social media.
There are several signs of SUD. Behavioral signs of SUD include:
- Relationship deterioration
- Acting suspiciously
- Ignoring responsibilities
- Sudden changes in relationships and hobbies
- Avoiding enjoyable activities to use drugs
- Using substances without regard for consequences
- Using substances to avoid withdrawal symptoms
- Heavily relying on a substance for normal functions
Physical signs of SUD
- Personal grooming or appearances are worsening
- Constant runny nose
- Extreme weight loss or weight gain
- Increase or lack of appetite
- Changing sleep patterns
- Pupils are drastically bigger or smaller than usual
- Slurred speech
- Weakened coordination
Psychological signs of SUD
- Anxiety
- Paranoia
- Fear
- Nervousness
- Lack of motivation
- Fast-changing mood swings
- Angry outbursts
- Personality changes
Conclusion
Veterans suffering in the quagmire of post-traumatic stress disorder compounded by alcohol or drug abuse can get the help they need to get sober and cope with life’s challenges. Many of the services available to struggling veterans are free. And the providers will respect your privacy.
You served your country. Now let your country serve you.
 Alternative to Meds Center, which offers drug-free treatment to help get veterans on the right track. The ATMC uses lab testing to determine physiological reasons for why guests may abuse alcohol. Therefore, the ATMC can tailor each program for each guest’s physiological needs. Call (888) 906-1547.
Alternative to Meds Center, which offers drug-free treatment to help get veterans on the right track. The ATMC uses lab testing to determine physiological reasons for why guests may abuse alcohol. Therefore, the ATMC can tailor each program for each guest’s physiological needs. Call (888) 906-1547.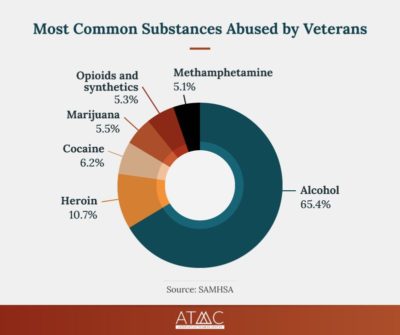 As mentioned, active-duty service members are more likely to abuse alcohol. Heavy drinking often carries over among veterans because of the addictive nature of alcohol.
As mentioned, active-duty service members are more likely to abuse alcohol. Heavy drinking often carries over among veterans because of the addictive nature of alcohol. Substance abuse and addiction, in general, can fall into more than one category.
Substance abuse and addiction, in general, can fall into more than one category.