TABLE OF CONTENTS
- The Goals of This White Paper
- An Overview of How Medication Addiction Happens
- Neuroadaptation and Addiction
- Addictive Biochemistry and Neuroadaptation Partner in Dependency
- Neuroadaptive Effects of Medications
- Addictive Biochemistry of Benzodiazepine Use
- Chief Complaint: Anxiety
- Contributing Factors to Benzodiazepine Use
- Excito-Toxic Poisoning
- Effects of Excito-Toxic Poisoning
- Findings from ATMC Heavy Metal Studies
- How Mercury Unburdening Changes Patient Health
- Mercury Converse to Dental Health
- Mercury, Chelation, and Benzodiazepine Dependency Conclusions
- Natural Benzodiazepine Alternatives
- Serotonin Pathway Natural Benzodiazepine Alternatives
- Other Natural Benzodiazepine Alternatives
- Medication Benzodiazepine Alternatives
- Gabapentin
- Benzodiazepine Cross-Over to Valium
- Sources
1 The Goals of This White Paper
ATMC BENZODIAZEPINE
ALTERNATIVES WHITE PAPER
In this white paper, you will find a unique and comprehensive cache of information covering the subject of benzodiazepines and the need for effective alternatives to using the prescription drug. The foregoing data comes from the perspective of an author who has been working with patients for 13 years to help reduce and eliminate their benzodiazepine dependence.
The researchers and medical practitioners at Alternative to Meds Center know there is a better way to deal with physical and mental health conditions, other than chemical dependency of traditional medicines. This white paper addresses the health risks of benzodiazepine use, explains how dependence develops and the impact on the human body and the mind. In addition, we reveal the many benzodiazepine alternatives available that help ease anxiety, other mental health conditions, and also better support the body’s natural systems for overall balance and wellbeing.
What to Expect
The benzodiazepine alternatives mentioned throughout this white paper include various products and, in many cases, a number of processes. To better understand the processes, we will cover basic mechanisms, technical mechanisms, and informative conversations that exist in more eclectic scientific fields such as environmental medicine. Should you want to go directly to the benzodiazepine alternatives, you may scroll towards the end of this paper where they will be summarized for your easy access.
Drawing from all of the data that Alternative to Meds Center has compiled over the course of the last 13 years, clearly, benzodiazepines is one of most difficult drug classes to undergo withdrawal from. In our experience, though there have certainly been exceptions, even heroin and other opiates are typically less complicated in comparison. Only antipsychotics have been more “addictive” as the neuroadaptation (dopamine receptor upregulation) from antipsychotics may cause a withdrawal mania or other hyper-excitability that can be difficult to manage. Those mechanisms are detailed in several of our medication resource pages such as Zyprexa withdrawal.
2 An Overview of How Medication Addiction Happens
AN OVERVIEW OF HOW MEDICATION ADDICTION HAPPENS
As a matter of definition, we would like to share a perspective on addiction.
When we think about “addiction”, what may first come to mind is some poor, fundamentally flawed person who is living fix to fix, leaving a pile of wreckage so high that they’d rather keep using than deal with it. This common stereotypical image may include the idea that addiction and all its’ repercussions are the person’s fault. Yet, the person addicted to substances will blame it on everyone else. While there may be elements of truth to this perspective, we consider it extremely myopic. Instead, we offer the notion of an addictive biochemistry as a primary cause for drug use.
Addictive biochemistry is a compelling and complex set of physiological and biological forces that may pull the user towards a particular substance for the purpose of finding relief. This addictive biochemistry is specific to the individual and is based upon patterning from genetics, diet, lifestyle, and psychosocial imprinting.
Certain people are pulled towards sedatives, others towards opiates, some towards alcohol, and yet others towards stimulants. We believe that if we establish a biological basis for these cravings, these can largely be corrected. This biological force can be the manifestation of mental torment that results in a physiological shift, as demonstrated in cases of PTSD. There are many physiological make-ups, traumas, and reward patterning that will manufacture or result in a chemistry shift and therefore, an addictive biochemistry.
3 Neuroadaptation and Addiction
Neuroadaptation and Addiction
From a physiological perspective, drugs tend to create neuroadaptation which can present in two ways: downregulation and upregulation.
Downregulation
In the process of downregulation, receptors become less receptive to the drug and; therefore, less receptive to the naturally occurring neurotransmitter that the drug is mimicking. Or in layman’s terms, the neurotransmitter that the drug was spending is spent and there is no more left to spend. When this occurs, the drug stops working or its efficacy is turned off. Either way, the drug is incapable of having the intended effect to the degree anticipated or desired by the user.
Upregulation
When the presence of a drug holds back the expression of a natural neurochemical, as seen with antipsychotics and the restriction of dopamine, upregulation occurs. This receptor starvation enhances receptivity of that receptor. In other words, when that receptor contacts the neurochemical being withheld, the reaction is much more pronounced. When the very drug that was holding back a particular neurochemical gets taken away, that neurochemical floods the synapse making contact with highly receptive receptors. There will then be a withdrawal reaction, expected, with an excess of that particular neurochemical.
In the case of pulling away an antipsychotic, a rebound of dopamine excess generally takes place. This phenomenon often gets confused with a resurgence of the original diagnosis. Usually, drugs act on more than one pathway. As such, there can be a barrage of chemical effects happening during a medication withdrawal.
4 Addictive Biochemistry and Neuroadaptation Partner in Dependency
Addictive Biochemistry
and Neuroadaptation Partner
in Dependency
Addiction, at least in part, is this neuroadaptation. Addictive biochemistry puts a person on the path to dependence, while the adaptive effects lock the doors.
Science shows us that the withdrawal effects of a medication or drug will, at a minimum, last until this neuroadaptation re-regulates itself. So, can a person be addicted to an antidepressant, benzo or an antipsychotic? Yes, if they cannot find the strength to surmount the winding path back through the neuroadaptive changes, without formidable consequences.
Some are inclined to give consideration to those people who need drugs, based on their current state of health, or imbalance. And we will not argue that there are people who find life easier and more manageable with medications than without, which is a personal choice.
Here, we are speaking more about the physiological withdrawal manifestations that exist outside of what an individual’s baseline drug-free disposition may be. And, if those physiological manifestations of withdrawal and pain from re-adaptation of the nervous system is perpetuating drug use, then that person could arguably be considered addicted.

5 Neuroadaptive Effects of Medications
Neuroadaptive Effects
of Medications
There are neuroadaptive effects from medications that lie outside of any other contributing factors, and can be influenced by genetics. We’ve studied this extensively and have published our findings here. During medication withdrawal, these neuroadaptive effects and the time needed to readjust back to baseline can be attended to, making the experience much more tolerable in the vast majority of persons wanting to reduce or remove their drug dependency. However, these neuroadaptive expressions can be very pronounced in symptomatology.
In mainstream viewpoint, confusion often exists between this neuroadaptive period versus attributing these expressions to a resurgence of a person’s underlying diagnosis.
It is important to note that any person would, to a varying degree, likely suffer neuroadaptive symptomatology if they were suddenly stripped of a medication that they had become adjusted to. This would be the case whether or not they had an underlying “diagnosis” in the first place. Just as if any of us imbibed alcohol or engaged in recreational drug use for a long period of time, the reverberations of that use would endure well past the time that the substance had effectively cleared our system.
Psychiatric medications operate by similar principles. At times, they create even more concerns when considering their neuroadaptive effects.
The “addictive biochemistry”, or the predisposing factors that led an individual to a particular medication or substance, can generally be attended to by softening the urge to self-medicate. These are the factors that were extant prior to medication use and will be the factors that will likely exist even after the re-neuroadaptation period has subsided.
How we can mitigate these factors with benzodiazepine alternatives is in further detail, below.
6 Addictive Biochemistry of Benzodiazepine Use
Addictive Biochemistry of Benzodiazepine Use
Obviously, a person would choose a benzo because they are trying to soften, reduce or eliminate a stimulus that is overwhelming them. The benzodiazepine mechanism of action is to make GABA, a naturally occurring inhibitory neurotransmitter, more highly expressed at the synapse.
In mainstream viewpoint, confusion often exists between this neuroadaptive period versus attributing these expressions to a resurgence of a person’s underlying diagnosis.
Anxiety, sleep disturbances, pain, anger, and muscle cramping are typical precursors prompting drug use. Anyone suffering to a point where life is untenable, for these reasons, might be expected to consider a sedative. The driving urge to balance overstimulation would be the addictive biochemistry and, in this case, the etiology of benzodiazepine use.
Differential Diagnosis
When a doctor is first investigating the concerns of a patient, the initial process includes asking some historical questions. When a chief complaint of anxiety is communicated, there are a few delineating questions that will assist the doctor in drilling down toward what may be causing the problem.

7 Chief Complaint: Anxiety
Chief Complaint: Anxiety
Patient ‘A’ expresses personal suffering due to anxiety. Although generally, a doctor will ask a number of significant questions, we would like to highlight the following:
- Is the onset sudden or gradual?
- Is the timing constant or intermittent?
In regards to timing, there is a big difference between a symptom that is happening constantly and one that comes and goes. The person with anxiety that comes and goes is often easier to correlate to a certain variable, and therefore remedy.
In contrast, constant anxiety that is like a background roar in the nervous system may waver in intensity but is predominantly there. Constant anxiety dispositions are generally more challenging and are most often associated with a neurotoxic body burden of heavy metals, pesticides, or other accumulations of excito-toxic havoc.
Excito-toxic means that foreign chemicals present in the nervous system overstimulate the nerve cells (neurons), even to the point of killing the neuron. In our experience, this body burden needs to be addressed before the individual can experience full relief without medications.
A large basis of the Alternative to Meds Center program involves alleviating this body burden
A person who is experiencing intermittent anxiety could have situational anxiety, such as when they are around people or circumstances that tend to stress them out. Other factors may indicate improper diet, blood sugar issues, or food allergies.
Very commonly, it is the drugs themselves that create a problem, known as interdosing withdrawal. This is evident when a person goes into withdrawal between medication dosings, most often seen with shorter-acting benzos, such as Xanax or Ativan. If the height of the withdrawal is occurring just prior to a scheduled dosing, this interdosing withdrawal phenomenon is likely involved. In addition, certain genetic situations may be involved in those with an intermittent anxiety disposition.
Find more about interdosing withdrawal here.
8 Contributing Factors to Benzodiazepine Use
Contributing Factors
to Benzodiazepine Use
Usually, a person will have a combination of contributors involved in benzodiazepine dependency. A combination of genetic impairment, a toxic body burden, and lifestyle contributors are common. For the purposes of discussion and detailed understanding, we address them below.
The GAD Genetic Polymorphism
The mechanism behind the GAD polymorphism is that the GABA is made from glutamate being exposed to the enzyme glutamic acid decarboxylase (GAD). Glutamate is the most excitatory neurotransmitter of the central nervous system, while GABA is the most inhibitory. Persons with the GAD genetic polymorphism may not be able to process as much GABA from glutamate. By design, this is unusual as the body tends to favor mechanisms that are easier to balance. However, the GAD polymorphism could be an advantage for those who balance a lot of activity in their life. However, in those with other contributing factors, this higher stimulation could tip over to anxiety.
Persons with this gene may have paradoxical reactions to GABA products, including natural GABA supplements, gabapentin, or the supplement Phenibut. While the aforementioned are typically favored over a benzodiazepine, in persons with the GAD polymorphism, these could cause more anxiety. In fact, GABA can actually reverse engineer back to glutamate 3,8. We suspect that this is accentuated in those with the GAD polymorphism.
This GAD correlation and theory is based upon a limited sample size and is only being presented here as a possible mechanism for paradoxical reactions.
GABA products are generally one of the most viable bridges away from benzodiazepines and the paradoxical reactions are comparably uncommon. But they do happen. Sometimes, if the person
reduces foods containing glutamate, they can better tolerate a GABA product. In these cases of paradoxical GABA reactions, other non-GABA benzodiazepine alternatives would likely be the favored treatment.
This genetic disposition may present as an anxiety that has more or less always been with the person, yet can come and go (intermittent).
But the anxiety can tend towards constant if the person is doing something that tips off the expression of this gene on a regular basis. Usually, this malady can be affected negatively by the consumption of foods containing glutamate, so a person eating glutamate foods regularly would present with more of constant anxiety, though they have possibly experienced times of relief.
Genetic contributors are not always the smoking gun we wish them to be. We have seen someone with, what could be considered, near ideal genetics suffering immensely; and others, with what would be considered a compromised “genetic hand” functioning normally.

9 Excito-Toxic Poisoning
Excito-Toxic Poisoning
On the level of the synapse, there is a mechanism that determines how nerve conduction and stimulation occurs.
For instance, acetylcholine is a neurochemical involved with muscle contraction. When acetylcholine is released into the space where one nerve talks to another, (the synapse), sodium channels open and allow for an electrical shift that results in nerve conduction. When the nerve meets the muscle (neuromuscular junction), muscle contraction occurs. Once the muscle contracts, an enzyme called acetylcholinesterase is released to break down and recycle acetylcholine, allowing the muscle contraction to stop.
In Pesticides
Certain pesticides, such as organophosphates and organocarbamates, can poison the acetylcholinesterase enzyme leaving the sodium channels open. A constant depolarization will occur and unchecked muscle contractions. When an insect is exposed to these chemicals, for example, they have a seizure and die.
Humans have a somewhat comparative anatomy to grasshoppers in that we also use acetylcholine for muscle contraction. An accumulation of these poisons within our nervous system would, therefore, be highly suspect for similar dysregulation.
Refer to this pesticide acetylcholinesterase video for a more visual illustration of this concept. The grasshopper twitching at the end conveys what persons endure within their nervous system when excito-toxic poisoned.

In Foods
We know that organophosphate and carbamate pesticides are poisonous to mammals as well,9 yet we still allow these poisons to be dumped on our food. While we don’t need to state the obvious about fast food and the level of chemicals and preservatives within, what gives us greater cause for concern are our food sources that present to the public as healthy.
Watching a pregnant woman stroll thru the fruit aisles of the local grocery store, believing that her food choices are good for her and her baby, when in fact she is unwittingly choosing food doused with neurotoxic garbage, is part of the greater injustice. By merely choosing organic fruits and vegetables for your produce can reduce toxic intake by as much as 80 percent.
Other examples of excito-toxins include glutamate, aspartate, and cysteine when added to foods in an unnatural way. These amino acids are normally found in the breakdown of certain roteins, yet the food industry has concentrated them in products like MSG and aspartame, common in diet sodas. Much of this phenomenon is covered in the book Excitotoxins: The Taste That Kills by Russell L. Blaylock
IMPORTANT NOTE: If you want an organic fruit or vegetable, the PLU code number on the sticker attached to the item or on the bag containing it will begin with a 9.
10 Effects of Excito-Toxic Poisoning
Effects of Excito-Toxic Poisoning
Any neurotoxic substance that specifically locks the nervous system into overdrive is an excito-toxic poison. The symptoms can onset gradually, as in the cases of long-term exposure,
eventually reaching a certain tipping point where the body can no longer regulate itself and achieve balance. This gradual onset hitting a tipping point is similar for most situations of lifetime toxic body burden accumulation, including heavy metals and organic chemicals.
However, there are cases we have treated that had a rapid onset indicating a potent and generally recent exposure.
Rapid onset instances include exposure when:
- A man had his home tented for insect removal
- A woman was left swimming for hours in diesel fuel after her boat capsized
- An evangelistic Pastor was living in a mold-infested home
In the above-mentioned cases, the onset of debilitating anxiety was sudden. Whether sudden or gradual, the more common feature of excito-toxic poisoning is that it is unrelenting, affecting the person on a daily basis. There may be windows of relief, but the majority of the time they are in a state of fight-or-flight crisis.
Alternative to Meds Center recommends organic diets free of additives for all individuals and pets. Elimination of toxic additives is highly recommended for any person, especially if suffering from anxiety.
Heavy Metal Body Burden
Poisons, by definition, alter normal physiology. Some poisons are lethal, and others knock out certain physiological systems. Heavy metals typically create havoc because they atomically mimic essential minerals, yet may not perform the same function. Heavy metals have the capacity to displace but not functionally replace essential minerals. Minerals are involved in most physiological processes to some degree, and the alteration of these physiological functions can be far-reaching.
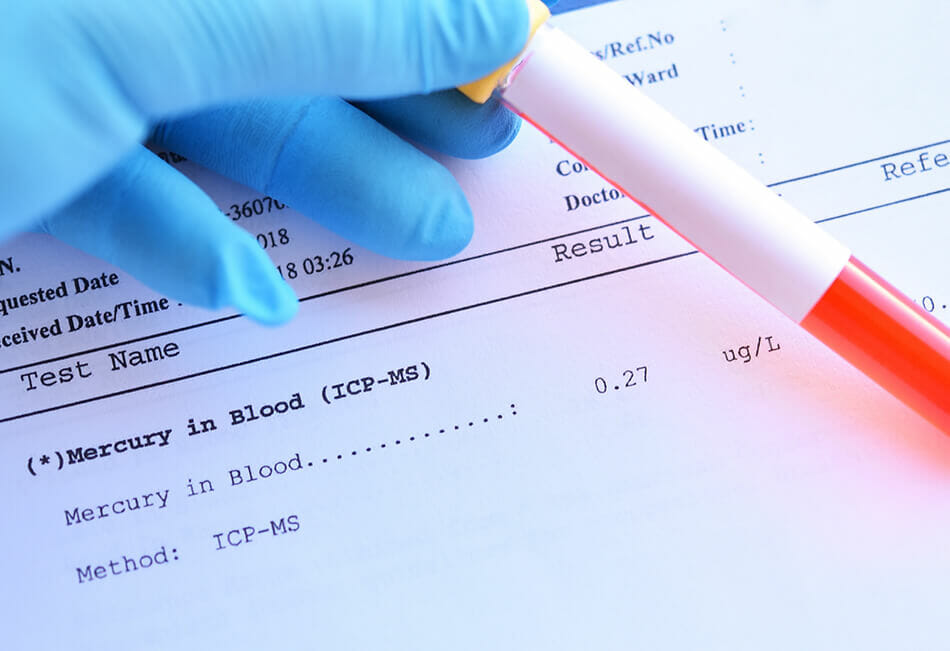
The Most Toxic Naturally Occurring Substance
For the purposes of benzodiazepine alternatives and anxiety dispositions, there is one heavy metal that we refer to as the king of chaos… mercury.
Mercury is the most toxic naturally occurring substance on the planet. The University of Calgary did an electron microscope study on neuronal degeneration in the presence of mercury. It clearly
nstrates how the tubulin fibers that create the structure of nerves literally fall apart in the presence10, 7 concentration of mercury, which is half of the EPA allowable limit for the environment.
11 Findings from ATMC Heavy Metal Studies
Findings from ATMC
Heavy Metal Studies
The Alternative to Meds Center has long held the belief that exposure to heavy metal toxins bears a strong role in a person’s self-perceived need to seek relief from symptomology through the use of medications. To further define our theory and provide proof, we have been performing heavy metal provocation studies, for nearly a decade, on a residential population.
The clinical observations are as follows:
- Elevated levels of mercury strongly associate with dispositions of anxiety, insomnia, and ruminating thoughts
- These symptoms are generally constant in disposition
- Over time, said symptoms are increasingly more debilitating
- Majority of study participants found substantial relief after addressing their toxic body burden
Mercury Disrupts Serotonin Synthesis
By applying the results of our case studies, we found that mercury interferes with the synthesis of serotonin. Serotonin is classically associated with the softening of anxiety, ruminations and assisting in sleep. Melatonin (the sleep neurohormone) is synthesized from serotonin. Persons with a mercury burden (combined with an essential mineral deficiency) generally do not utilize 5HTP, tryptophan or melatonin supplementation well enough to offset their symptoms. Although a small population of people, at times, finds these products curiously stimulating, those without a mercury burden typically receive the intended effect of sedation from these types of supplements.
As often happens in clinical settings, an observation is made and then theories are generated to explain the observation. The observations are typically true, whereas the proffered explanations may or may not be true. As we are largely in uncharted territory, through the ATMC case studies and ongoing treatment protocols of our patients suffering with toxic body burden, we offer this information as an explanation for the phenomenon that has been repeatedly demonstrated in our Center.
12 How Mercury Unburdening Changes Patient Health
How Mercury Unburdening
Changes Patient Health
We have found that persons with a mercury burden and the symptoms of unrelenting anxiety, ruminating thoughts and insomnia, typically do not find relief until they have addressed the mercury burden.
Mercury unburdening, even with chelation, is a lengthy process that generally entails treatment for up to three months before patients experience enough relief to believe it is working. A person typically will go from having constant anxiety to having a “few good days” within that time. As treatment continues, there are more good days reported than bad, and so on. This slow path back to wellness is the unfortunate reality for most of our patients harboring a mercury burden in conjunction with the aforementioned constant anxiety, insomnia, and ruminating thoughts trio.
13 Mercury Converse to Dental Health
Mercury Converse to Dental Health
We encountered two persons who found immediate relief from severe symptomatology after having their mercury fillings removed.
We surmised that perhaps the metals in the mouth created some sort of electrical or ionic influence on acupuncture meridians in the tooth sockets. This was the viewpoint of the late Dr. Hal Huggins, a dentist, who pioneered the perspective that mercury fillings should be outlawed. Again, the observations were correct, as these two people enjoyed immediate relief from extremely debilitating, long-term symptomatology. However at this juncture, we can only guess at the mechanism.
Understanding Mercury Chelation
We have found substantial evidence that persons undergoing mercury chelation treatment and remineralization for constant anxiety, rumination, and insomnia tend to get sustainable relief. Conversely, there are those patients while under our care who chose not to do the chelation because of negative perceptions about chelation that they had read or heard elsewhere. And it was not uncommon for members of that group to fail to enjoy lasting and substantial symptomatic relief.
There are other methods of mercury removal besides chelation but those methods tend to take even longer. At ATMC, we use an oral form, testing the individual for reaction with a minimal test dose. As of the writing of this paper, none of our patients have experienced adverse reactions to chelation that were a cause for concern. We also are very diligent around mineralization as chelation pulls minerals as well as metals. And so it is very important to replace the minerals lost in the chelation process.
14 Mercury, Chelation, and Benzodiazepine Dependency Conclusions
Mercury, Chelation, and Benzodiazepine Dependency Conclusions
Through more than 13 years of researching toxic body burden and its relation to physiological and emotional wellbeing in our patients, Alternative to Meds Center has formulated the following conclusions:
- Persons whose symptoms are being caused by a mercury burden typically need to relieve that burden in order to find relief.
- Additionally, persons in this category may not be able to substantially reduce or eliminate benzodiazepine use, until that burden has been attended to sufficiently.
Note that statement #2 may appear disheartening but is not meant as a statement of fact for all persons in this situation. The reality of the effects of mercury exposure and associated treatment needs are best when considered on a case by case basis.
For example, when a person is not sleeping or eating, their existence can easily become an anxious, ruminating mess. Physiological detox requires at least some degree of sleep, eating and other basics, in order to be effective or even safe for that matter. The best course of action may be to leverage the stability that does exist, and apply it toward therapies that will relieve the toxic burden first. Once they achieve substantial relief, it is then easier to focus on benzodiazepine medication withdrawal efforts.
15 Natural Benzodiazepine Alternatives
Natural Benzodiazepine Alternatives
People who are coming off of benzodiazepines are typically well advised to assist the process with supplementation. The theory and observations are that if you support the inhibitory aspects of the nervous system, you can alleviate depletions and ease the withdrawal.
Unfortunately, there is a substantial portion of people experiencing benzodiazepine withdrawal who will only marginally benefit by supplementation alone.
People with toxic pathways from heavy metals and other accumulated poisons tend to get far less benefit from supplements. This is because the supplements are trying to work the same pathways that are impaired. We have found that efforts to clear these pathways in conjunction with supplementation are much more effective. However, there are some people who will have a paradoxical reaction to aspects meant to assist in sedation and instead, get stimulated by them. It is in these persons that pathway impairment is suspect.
GABA Pathway Natural Benzodiazepine Alternatives
GABA, an inhibitory neurotransmitter, is the main neurotransmitter involved in benzodiazepine metabolism. There are a number of natural GABA supplements available on the market. These products tend to have a noticeable effect when tested on persons not suffering from extreme anxiety. Unfortunately, they are largely muted in effect and fall short of being a stand-alone replacement during a benzodiazepine transition. The absorption from an oral form and realized improvement to brain levels seems to be limited. This is why ATMC uses a sublingual nanonized spray (under the tongue) that assists with bioavailability and absorption.
Taurine is an amino acid very similar to GABA and glycine. Taurine can activate GABA receptors and is useful for anxiety relief. Typically, taurine would be used with GABA and glycine to form a synergistic effect to help bolster the inhibitory neurotransmitters. Though we have seen few, if any, paradoxical stimulations when inducting taurine, there is some literature that indicates it can raise brain concentrations of glutamate1 which could be problematic for anxiety dispositions, particularly those with the GAD polymorphism.
16 Serotonin Pathway Natural Benzodiazepine Alternatives
Serotonin Pathway Natural Benzodiazepine Alternatives
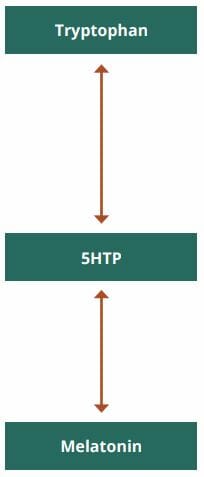
5HTP is the next step in the biochemical process where tryptophan is converted into 5HTP and then later into serotonin. 5HTP is generally a good benzodiazepine alternative but has produced the paradoxical effect of excitability in at least 10 percent and as much as 20 percent of those withdrawing from benzodiazepines. For this reason, we tend to favor tryptophan.
Melatonin is the neurohormone that the body uses to induce sleep. It is made from serotonin. Unfortunately, melatonin is broken down during the digestive process and is ultimately converted into tryptophan to exit the gut and get into the bloodstream. It will then form 5HTP and then only within the brain, can it convert to serotonin and then melatonin. Thus, it would stand to reason that if melatonin helps with insomnia, a person most likely does not have impairment of this pathway. Conversely, if melatonin is ineffective, or if there is a paradoxical reaction of excitability, then quite possibly there is a blockage. We refer to this as the melatonin challenge. And though it is not diagnostic, it does lead us to investigate areas of neurotoxic poisoning.
17 Other Natural Benzodiazepine Alternatives
Other Natural Benzodiazepine Alternatives
CBD, or cannabidiol, is a diverse set of molecules and active metabolites. When ingested, they
converge with varying individual metabolism genetics, and can benefit how they utilize those molecules and active metabolites. CBD seems to have a rather indirect effect on the NMDA receptor, rather than a direct one, and also has shown the ability to enhance the inhibitory neurotransmitter glycine.5 We prefer the nanoemulsified CBD hemp products, such as those used by Quicksilver.
Other products tend to require 2 to 3 times the suggested dosing level to get the intended effect. This may likely be the administration of choice for those with the GAD polymorphism who also react poorly to GABA, glycine, taurine or gabapentin, as not everyone with a GAD genetic marker will react poorly to GABA, glycine, taurine or gabapentin.
Theanine is found in green tea, and is typically a very good benzodiazepine alternative as the majority of its action seems to be in the blocking of the excitability of glutamate at the NMDA receptor. Also known as 5-N-ethylglutamine, theanine is structurally very similar to glutamate and can, in some persons, have stimulating effects very similar to glutamate. In most, the inhibitory effects of L-theanine are much more noticeable than the excitatory ones, but it is something to consider when using it as a benzodiazepine alternative.
Inositol taken at a 12-18 gram dose (a big dose) has been shown to significantly reduce panic attacks, anxiety, and OCD.7 Inositol is generally considered as safe to consume. Inositol is likely involved in the reverse desensitization of serotonin receptors and has an efficacy on par with antidepressants for OCD, without the toxic side-effects.6

Glutathione is the body’s main antioxidant. Since so many of the reasons why a person is put on benzodiazepines are the result of underlying neurotoxic poisoning, clearing up that burden is a must. We highly recommend that our patients undergo glutathione treatment at the Center, usually with a liposomal formulation (fat soluble) or nebulization (breathing a vaporized administration).
There is an entire company designed around the use of whey products containing glutathione precursors for the purposes of benzodiazepine withdrawal. If a person’s genetics are geared toward
the low output of glutathione from the amino acids that combine to form it, we suspect that adding
more glutathione precursors may have a muted effect. Hence, our preference is for more direct
administrations, such as liposomal or nebulization.
The majority of those who react poorly to glutathione tend to be sulfur sensitive. Therefore, those who are sensitive to sulfur should approach nebulization with caution. (Please note: sulfur sensitive is different than Sulfa). Those who do react are, at times, found to have a genetic polymorphism called the CBS upregulation. Reactions usually present as a mild asthma attack from the nebulization. For this reason, the first administration should be to test first, using only a couple inspirations with the product.

Valerian Root has shown positive effects for those amidst benzodiazepine withdrawal. A Brazilian team studying the effects of Valerian root for those withdrawing from benzodiazepines demonstrated positive results on sleep.2 While valerian root did not assist in the onset of sleep, it did seem to improve the quality of sleep without any noted interactions with the medications. It was a small study of 19 persons using lower end dosing ranges.
Glycine is like GABA, a potent inhibitory neurotransmitter. While GABA is the main neurotransmitter of the CNS, glycine is most prevalent in the brainstem and spinal cord. For most, glycine is a wonderful adjunct and benzodiazepine alternative. Curiously, glycine can also increase the binding ability of glutamate to the NMDA receptor, meaning that glycine can be both excitatory and inhibitory within the CNS. And thus, there are going to be those few who get more stimulation from glycine than sedation. In our experience, it has been very, very few. It should be considered that it is often those few who are differently wired that present with the most pronounced problems. In these patients, we introduce other possibilities in the interest of helping them navigate these differences.
Magnesium is vital to calcium ions in the body. Benzodiazepines have an effect on calcium channels and may, in part, be why benzos act as muscle relaxants. When a person is rapidly coming off of a benzodiazepine, there can be a sudden influx of calcium ions that could cause a seizure. Magnesium helps to counterbalance calcium and typically acts as a calming agent, instrumental to those seeking benzo alternatives.

18 Medication Benzodiazepine Alternatives
Medication Benzodiazepine Alternatives
All matters within this paper, specifically conversations regarding medications and supplements, need to be talked about with your medical provider before attempting.
Gabapentin is typically a good bridge drug for coming off of benzodiazepines. Gabapentin is generally going to require a higher milligram dosing to achieve benzodiazepine equivalence. Basically, gabapentin is a GABA analog and is not too far removed from the amino acids leucine and isoleucine.
One of the methods of action of benzodiazepines is to make GABA more effective at the synapse. However, benzos do not make GABA. In essence, benzodiazepines exhaust the GABA pathways. Gabapentin has the ability to raise GABA concentrations within the CNS.4 And gabapentin does not require the liver to detoxify it, like most drugs, making it much less impactful than benzodiazepine toxicity. Gabapentin does transfer more GABA into the CNS than what would be expected through supplementation. So the problems of downregulation to the drug and neuroadaptation are likely at play.
Our experience with gabapentin shows us that for the vast majority of patients, it is well tolerated. It seems as if many benzo users are GABA depleted and even a lower dose can have a strong sedating effect. This is a good sign when considering a temporary benzodiazepine alternative bridge. There are those few who have a stimulating effect from gabapentin, and the GAD polymorphism is suspect in these patients.
19 Gabapentin Caution
Gabapentin
Is gabapentin addictive?
Any drug can be addictive. Gabapentin is likely on the lowest rung of drugs in the respect of toxicity and addictiveness, and withdrawing from it is almost certainly easier than benzodiazepine detox. For many, it may be a highly useful step-down on the path to being benzodiazepine medication-free. Most persons have a much, much easier time coming off of gabapentin than they were having with the benzos and with far fewer side effects.
It is pragmatic to slowly introduce gabapentin as the benzodiazepine is being reduced. Gabapentin has a short half-life and may have to be prescribed 3 to 4 times a day during the process so that the patient does not experience inter-dosing withdrawal.
There are those who will have a bad reaction to any drug. We encourage anyone who is reading this and has experienced adverse side effects due to medication use to contact your doctor and explain the circumstances. No two patients are the same, and a good doctor will listen to your experience and respect it.
Phenibut is technically β-phenyl-GABA and very similar to gabapentin. In other words, it is GABA with a phenyl group at the beta position of GABA. We have put it under the “drug medication”
heading even though it is technically not licensed as a drug and is available without a prescription.
It can be a helpful bridge, is generally well tolerated, but can have an addictive backbite though generally far less so than a benzodiazepine. When used as a bridge for getting off of benzos, it can be effective. As with gabapentin, Phenibut forces a GABA effect. Any drug or supplement that does this could be problematic.
20 Benzodiazepine Cross-Over to Valium
Benzodiazepine Cross-Over to Valium
This technique is one strategy for benzodiazepine withdrawal and is one of the favored treatments for persons who are trying this at home. The Alternative to Meds Center does not do outpatient treatment, and our inpatient treatment may use Valium or we may perform a direct tapering from the drug that is currently being used.
Please know that we are not advising what you should do and this information is being presented as an example, which you can share with your healthcare provider.
When a person is on a benzo that has a short half-life like Xanax, Ativan, or Klonopin, it may be pragmatic to convert over to a longer half-life medication. Generally, shorter half-life drugs have a sharper onset of withdrawal. This technique seeks to avoid that reality by implementing a softening of that phenomenon. As Valium leaves the body typically more slowly, the sharpness of withdrawal can be blunted enough to make the process tolerable.
Going straight from one benzo to Valium can have its complications and is likely not the best choice to do so. The patient may not metabolize Valium in the same way as the benzodiazepine that they were accustomed to. The sudden swap may be unnecessarily jarring. To alleviate this, Valium is slowly introduced, while the other short-acting benzo is slowly replaced. When the transition is complete, the person will be on a level of Valium that has an equivalency similar to the original drug.
Example: 3mg of Ativan is being taken in 1 mg dosings three times a day. The midday dose of Ativan may be reduced from 1 mg to .5 mg and also adding 5 mg of Valium at that time. The other doses stay at the same level of Ativan. If the initial induction is well tolerated, then the remaining doses can be attempted in a similar way, exchanging .5 mg Ativan for 5 mg Valium until the person is stable on 30 mg Valium
This slower transition method reduces the potential for problematic substitution reactions and lessens the potential for equivalency dosing errors.
This is just an example and the equivalency of 10 mg Valium to 1 mg Ativan is an approximation. For some doing this at home unsupported by other alternatives to benzodiazepines, this process may take months. It is really based upon the person.
The Alternative to Meds Center typically favors a direct tapering for those in residence largely because of time constraints. Our experience is that when combined with other considerations, direct tapering can be similarly effective. There are some situations where we use Valium crossovers, and there are some who have to relieve neurotoxic burden before they can even realistically endure medication reduction. Each situation has its own strategy.
How to Use Benzodiazepine Alternatives Information
All of the information in this white paper is just that, information – based on years of patient treatment experiences and associated case studies. We are not giving advice for what you should do at home as these are talking points to share with your healthcare provider. Making a decision to seek help for the gradual taper or removal of benzodiazepine dependency is best supported in a medically-supervised environment.
A method of treatment that is the salvation for one person could be highly detrimental to another person. This careful discernment from patient to patient is the reason why Alternative To Meds Center only offers inpatient services. Should you want to consider inpatient assistance for benzodiazepine drug dependence, please visit our website www.alternativetomeds.com and we will
provide a more informed assessment.
To get a better understanding of what we do at our Center and how we positively change the health outcomes of our patients every day, review the findings in our 2018 Case Study.

21 Sources
Sources:
- Effect of taurine on the concentrations of glutamate, GABA, glutamine and alanine in the rat striatum and hippocampus Proc West Pharmacol Soc. 2007;50:95-7. Molchanova SM1, Oja SS, Saransaari P.
- Can valerian improve the sleep of insomniacs after benzodiazepine withdrawal? Prog Neuropsychopharmacol Biol Psychiatry. 2002 Apr;26(3):539-45. Poyares DR, Guilleminault C, Ohayon MM, Tufik S.
- GABA and Glycine Steven M. Paul 2000
- The Impact of Gabapentin Administration on Brain GABA and Glutamate Concentrations Neuropsychopharmacology. 2012 Dec; 37(13): 2764–2771. Kejia Cai, Ravi PR Nanga, Lisa Lamprou, Claudia Schinstine, Mark Elliott, Hari Hariharan
- Endocannabinoid control of glutamate NMDA receptors: the therapeutic potential and consequences of dysfunction Oncotarget. 2016 Aug 23; 7(34): 55840–55862. María Rodríguez-Muñoz, Pilar Sánchez-Blázquez, Manuel Merlos, and Javier Garzón-Niño
- Controlled trials of inositol in psychiatry. Eur Neuropsychopharmacol. 1997 May;7(2):147-55. Levine J.
- Double-blind, placebo-controlled, crossover trial of inositol treatment for panic disorder. Am J Psychiatry. 1995 Jul;152(7):1084-6. Benjamin J, Levine J, Fux M, Aviv A, Levy D, Belmaker RH.
- How to Increase GABA and Balance Glutamate Holistic Help May 28, 2014 Cynthia Perkins
- Mechanism of action of organophosphorus and carbamate insecticides. Environ Health Perspect. 1990 Jul; 87: 245–254. T R Fukuto
Nothing on this Website is intended to be taken as medical advice. The information provided on the website is intended to encourage, not replace, direct patient-health professional relationships. Always consult with your doctor before altering your medications. Adding nutritional supplements may alter the effect of medication. Any medication changes should be done only after proper evaluation and under medical supervision.